Posted by: Northwest Eye in Dry Eye, General on August 1, 2025
Overview
The article on ‘Understanding Dry Eye Disease: Causes, Diagnosis, and Treatment’ compassionately addresses the multifaceted nature of dry eye disease. It details symptoms, underlying causes, diagnostic methods, and management strategies, acknowledging that many may feel overwhelmed by this condition.
We understand that effective treatment relies on recognizing both environmental and systemic factors contributing to dry eye disease. This includes employing a combination of:
- artificial tears
- prescription medications
- lifestyle modifications
to alleviate symptoms and improve your quality of life. We are here to help you through this process.
Introduction
Dry eye disease is a common yet often overlooked condition that can significantly impact daily life, causing discomfort and frustration for millions. We understand that dealing with this issue can be challenging.
Understanding the intricate web of causes—from environmental factors like low humidity and excessive screen time to systemic influences such as hormonal changes and autoimmune disorders—can empower you to take control of your eye health.
It’s common to feel overwhelmed by the many potential triggers and symptoms. But how can you effectively navigate the diagnosis and treatment landscape to find lasting relief?
We are here to help you through this process.
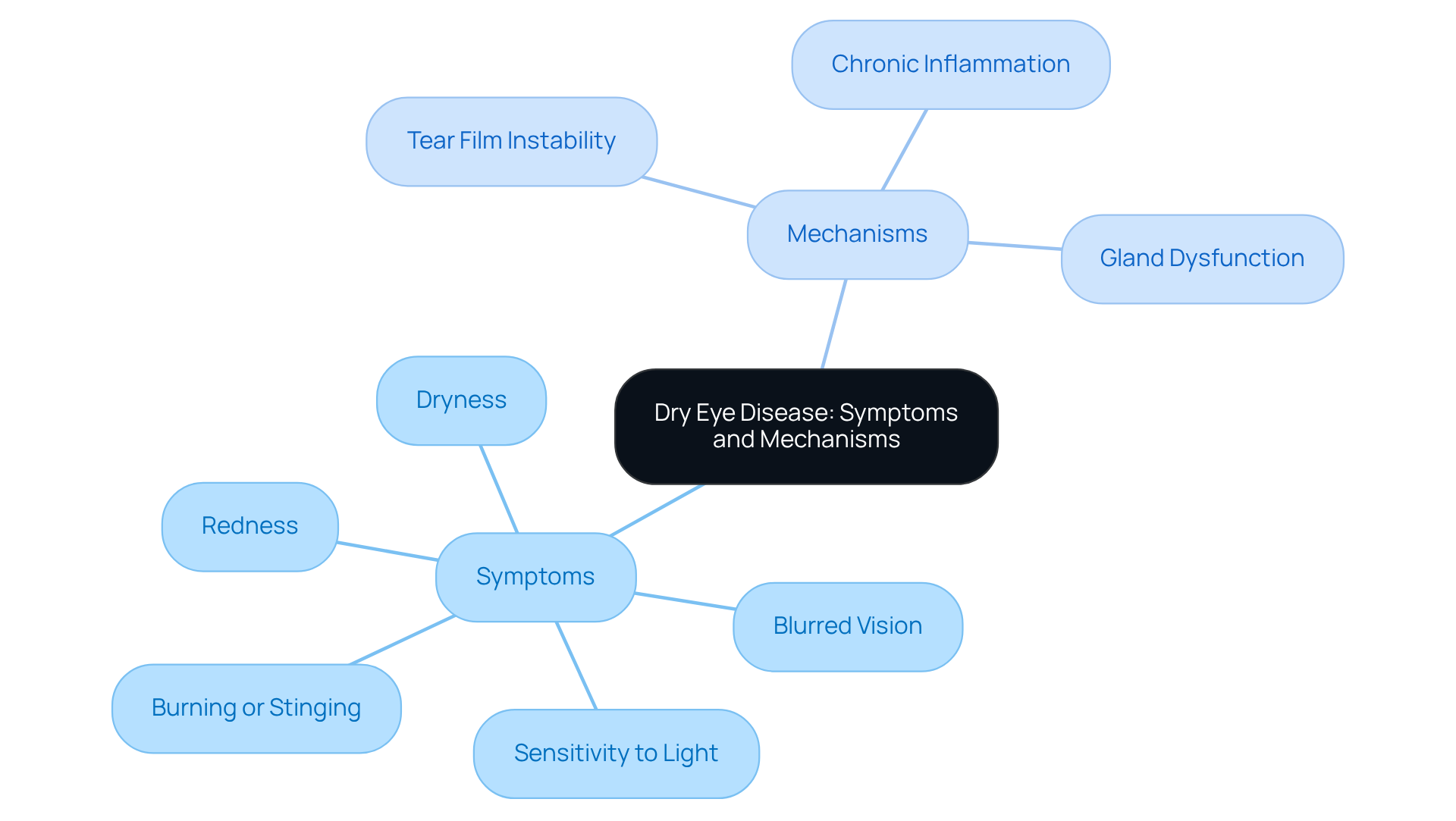
Define Dry Eye Disease: Symptoms and Mechanisms
Dry ocular condition occurs when your eyes do not produce enough moisture, or when the fluid evaporates too quickly. We understand how uncomfortable this can be. Symptoms may include:
- Dryness: A persistent feeling of dryness in your eyes.
- Burning or stinging: Discomfort that can be made worse by environmental factors.
- Redness: Inflammation of the eye surface.
- Sensitivity to light: Increased discomfort in bright environments.
- Blurred vision: Fluctuating clarity of vision, often improving with blinking.
The mechanisms behind dry eye disease involve several factors:
- Tear film instability: A disruption in the tear film can lead to inadequate lubrication.
- Dry eye disease: Chronic inflammation of the ocular surface can exacerbate your symptoms.
- Gland dysfunction: Meibomian gland dysfunction can decrease oil production, resulting in the increased evaporation of moisture that contributes to dry eye disease.
It’s common to feel frustrated with these symptoms, but know that support is available. We are here to help you through this process and provide the care you need.
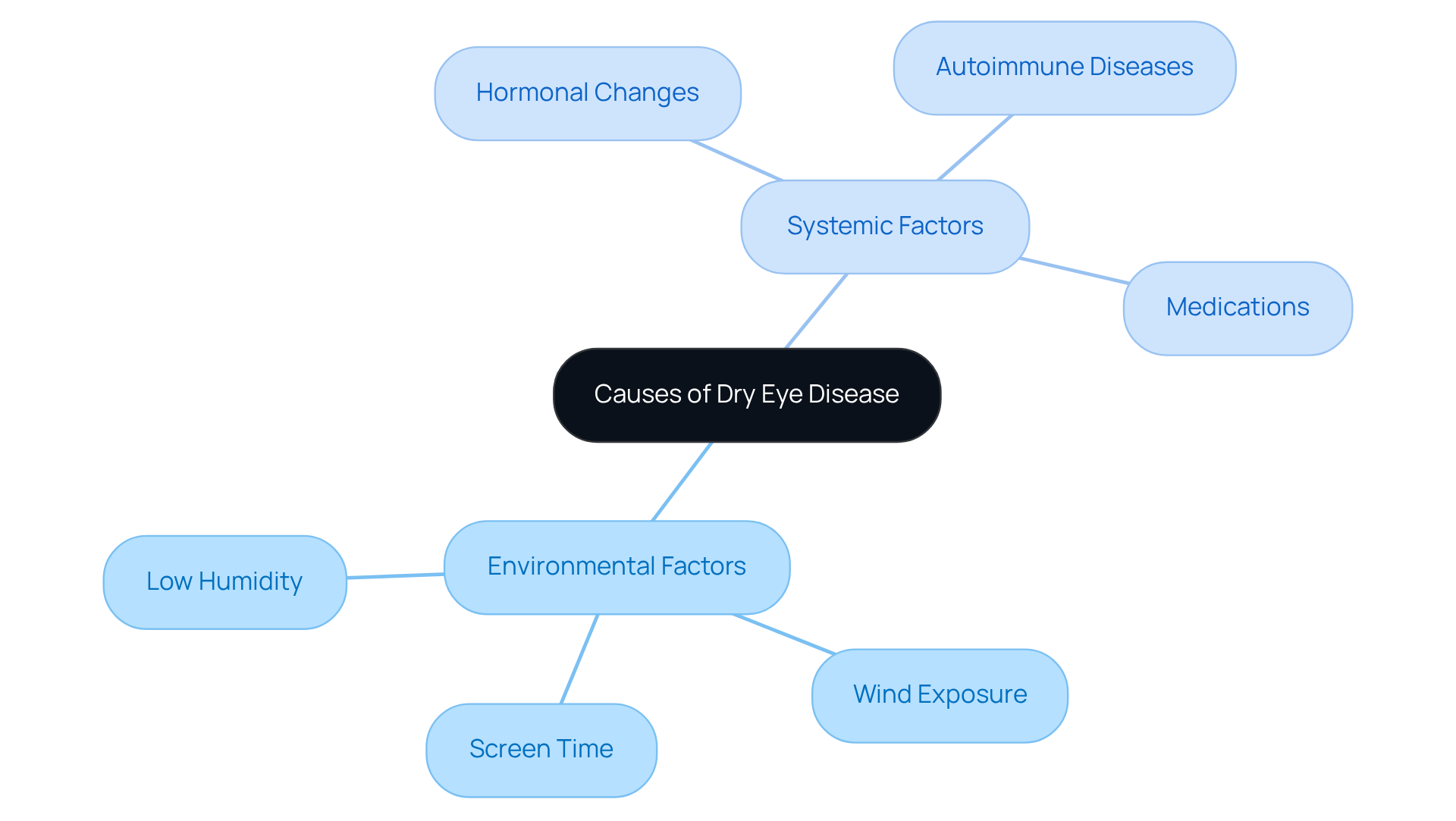
Explore Causes of Dry Eye: Environmental and Systemic Factors
Understanding the several factors that contribute to the development of dry eye disease can help you feel more empowered in managing your eye health. These factors can be categorized into environmental and systemic influences.
Environmental factors include:
- Low humidity: Dry air can accelerate tear evaporation, leading to discomfort. We understand how this can make daily activities challenging.
- Wind exposure: Windy conditions can worsen fluid loss, further intensifying issues. It’s common to feel the effects of the environment on your eyes.
- Screen time: Prolonged use of digital devices significantly reduces blink rates, which can lead to dryness. Research shows that extended screen time is linked to heightened dry eye disease, with a p-value of less than 0.001. This emphasizes the importance of taking regular breaks and practicing good eye care.
Systemic factors also play a crucial role:
- Hormonal changes: Conditions such as menopause can lead to decreased tear production, making women particularly susceptible to dry eye disease. Studies indicate that dry eye is common during menopause due to hormonal shifts, greatly affecting gland function.
- Autoimmune diseases: Conditions like Sjögren’s syndrome significantly impact tear gland function, leading to persistent dry eye issues. Statistically significant relationships have been identified between dry eye indicators and systemic rheumatologic diseases. Understanding these underlying conditions is vital for effective management.
- Medications: Certain medications, including antihistamines and antidepressants, are known to worsen dry eye conditions. Statistically significant connections exist between dry eye indications and the use of psychotropics, glucocorticosteroids, depression, diabetes, and allergies. We encourage patients to consult with their healthcare providers to identify any potential medication-related contributors to their condition.
Recognizing these factors is crucial for the effective management and treatment of dry eye disease. We are here to help you navigate this journey, empowering you to make informed decisions about your eye health.
Diagnose Dry Eye Disease: Assessment Techniques and Tools
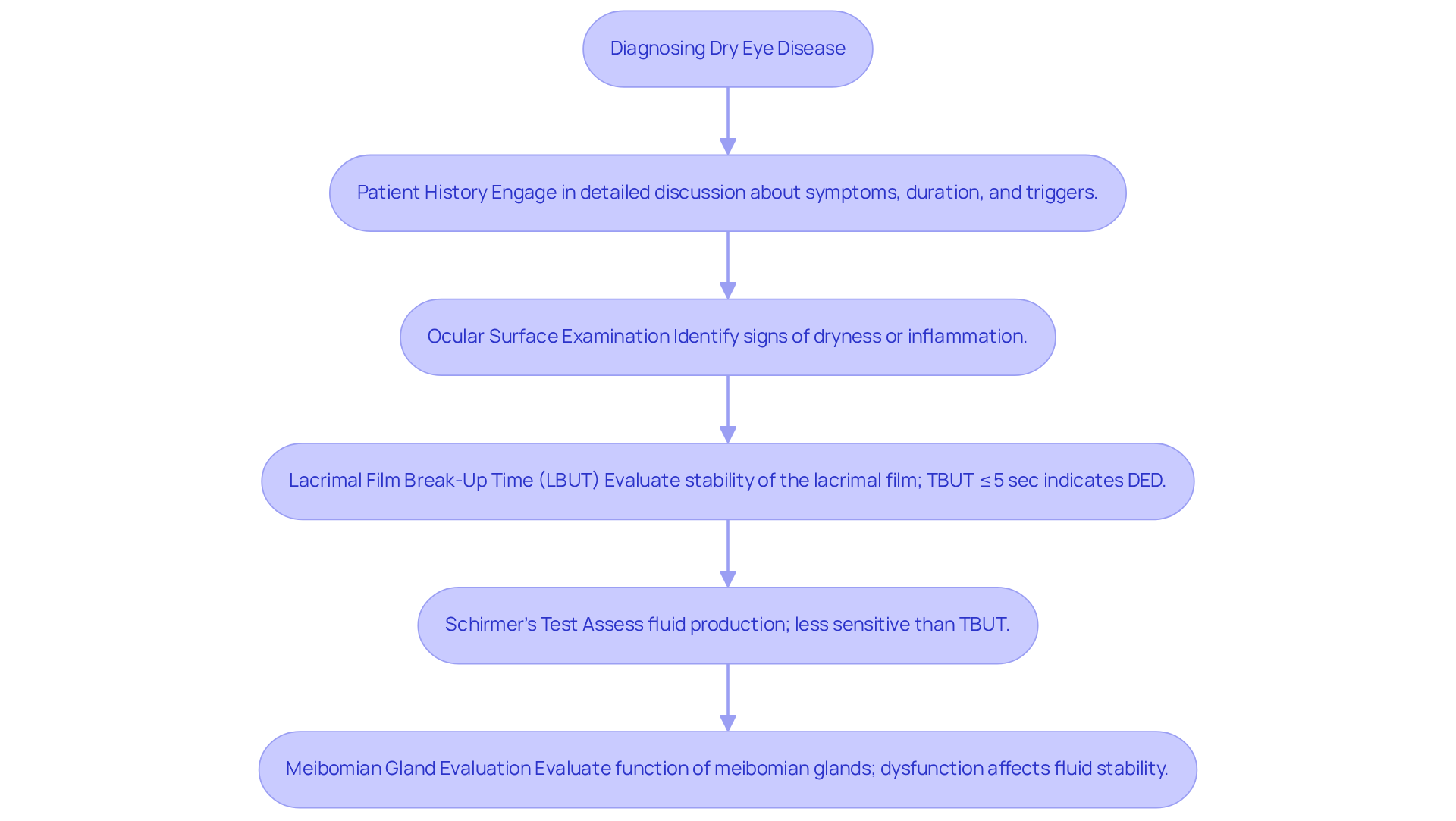
Diagnosing dry eye disease generally requires a comprehensive approach that integrates patient history with clinical assessments. We understand that this process can feel overwhelming, but it’s essential for accurate diagnosis. Here are the key components to consider:
- Patient History: Engaging in a detailed discussion about your symptoms, their duration, and potential triggers with your healthcare provider is crucial for accurate diagnosis. This conversation helps us understand your unique situation better.
- Ocular Surface Examination: A thorough examination of the eye’s surface allows us to identify signs of dryness or inflammation, which are common indicators of dry eye disease. It’s common to feel anxious about what this entails, but we are here to guide you.
- Lacrimal Film Break-Up Time (LBUT): This test evaluates the stability of the lacrimal film by assessing how quickly moisture evaporates from the eye’s surface. Recent studies indicate that a TBUT of 8 seconds or less is often linked with symptoms of dry eye disease. For many patients with dry eye disease, the average fluid breakup time is around 3.0 seconds, indicating severe dry eye disease at diagnosis.
- Schirmer’s Test: This test assesses fluid production by placing a small strip of paper in the lower eyelid. Research shows that TBUT has a significantly higher sensitivity for diagnosing dry eye disease compared to Schirmer’s test, with TBUT demonstrating an effectiveness rate of 87.3% in identifying dry eye disease, compared to 69.5% for Schirmer’s test. We recognize that these tests may sound intimidating, but they provide valuable insights into your condition.
- Meibomian Gland Evaluation: Evaluating the function of the meibomian glands, which generate the oily layer of moisture, is crucial. Meibomian gland dysfunction is found in over half of dry eye patients and significantly affects fluid stability, so understanding this aspect is vital.
Looking ahead to 2025, innovative evaluation instruments are emerging that enhance the diagnosis of dry eye disease. These noninvasive devices allow for dynamic analysis of the fluid film and visual clarity, offering a more thorough understanding of film instability, which is a fundamental mechanism in dry eye pathology. By utilizing these assessment techniques, healthcare providers can better tailor treatment strategies to meet your unique needs.
Additionally, it is important to note the newly discovered subtype of dry eye disease, the short breakup time-type (BUT), which is linked to ocular neuropathic pain and eye strain. We are here to help you through this process and ensure you receive the care and support you deserve.
Treat Dry Eye Disease: Comprehensive Management Strategies
Effectively managing dry eye disease requires a compassionate approach that takes into account the severity and underlying causes of your condition. We understand that dealing with dry eyes can be uncomfortable, and we are here to help you find relief through tailored strategies.
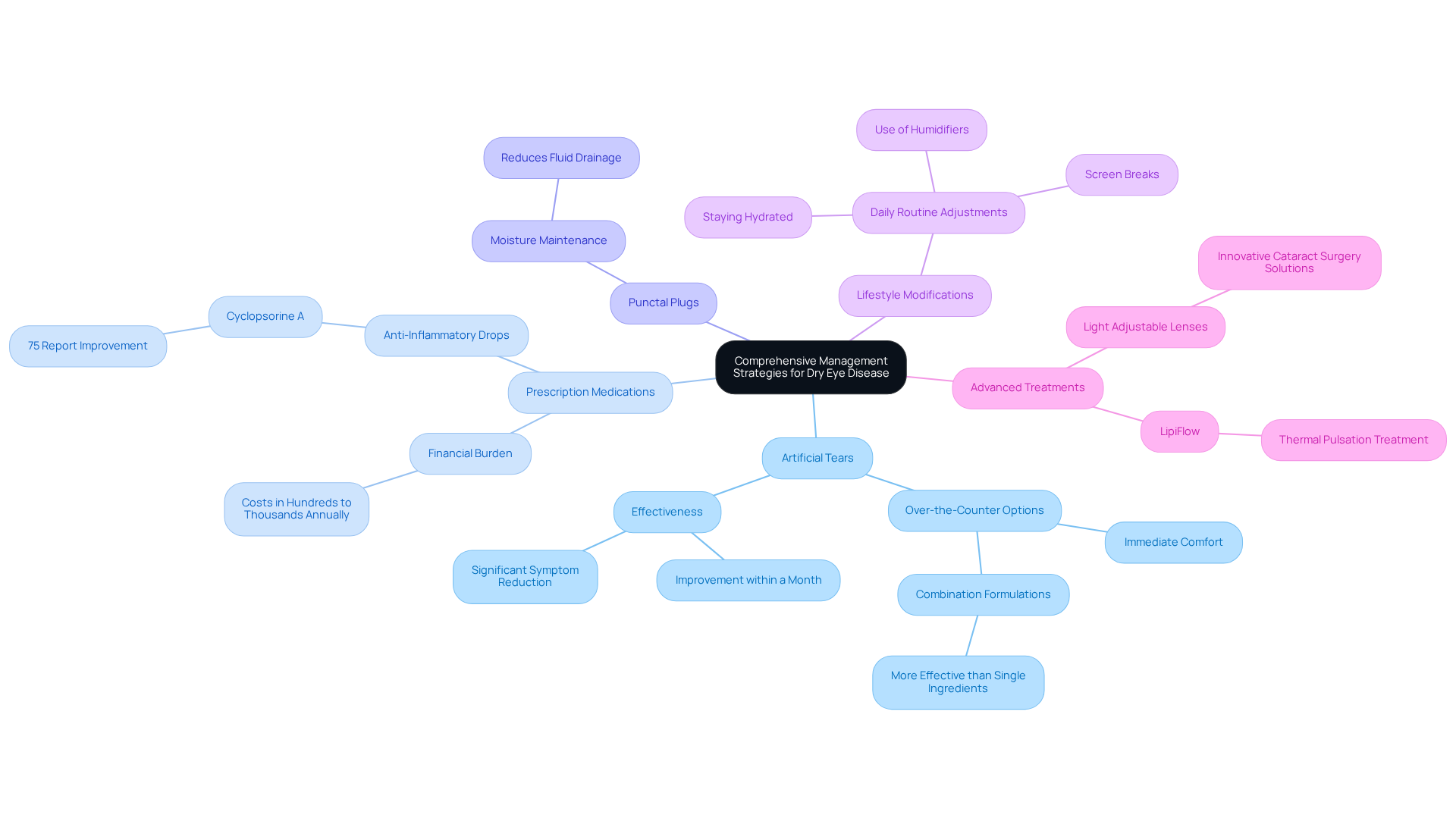
- Artificial Tears: Over-the-counter lubricating eye drops are often the first line of defense, providing immediate comfort for many. Research indicates that consistent use of synthetic eye drops can significantly alleviate discomfort within a month. Additionally, combined formulations frequently yield better outcomes than single-ingredient options. With nearly 16 million diagnosed cases of dry eye disease in the U.S., it’s clear that this condition affects many individuals just like you.
- For those with moderate to severe dry eye disease, prescription medications like anti-inflammatory drops such as cyclosporine A can be particularly effective in boosting fluid production. Approximately 75% of patients report meaningful symptom improvement with this treatment. However, we recognize that the financial burden of dry eye treatments can be substantial, often running into hundreds or even thousands of dollars each year.
- Punctal Plugs: These small devices can be a game-changer for maintaining moisture on the eye surface. By reducing fluid drainage, they offer relief for patients who may not find enough comfort from synthetic solutions alone.
- Lifestyle Modifications: Simple adjustments in your daily routine can make a significant difference. Taking regular breaks from screens, using humidifiers, and staying hydrated are essential steps, especially for those who spend long hours in dry or air-conditioned environments. We understand that these changes can be challenging, but they are vital for your comfort.
- Advanced Treatments: Innovative options like LipiFlow provide thermal pulsation treatment for meibomian gland dysfunction, a common cause of DED. Moreover, the use of Light Adjustable Lenses during cataract surgery showcases our commitment to utilizing cutting-edge solutions to enhance your experience and outcomes.
By combining these strategies, we aim to create a comprehensive approach to managing dry eye disease, ensuring that care is tailored to your unique needs. For example, a study evaluating artificial tears containing trehalose and hyaluronic acid in women aged 42-54 demonstrated significant symptom improvements, reinforcing the effectiveness of these treatment options. Remember, we are here to support you every step of the way.
Conclusion
Understanding dry eye disease is crucial for maintaining optimal eye health and comfort. We understand that this condition arises when the eyes fail to produce adequate moisture or when tears evaporate too quickly, leading to a range of uncomfortable symptoms, including dryness, burning, and blurred vision. By recognizing the underlying mechanisms and various contributing factors, individuals can take proactive steps towards managing their symptoms and improving their quality of life.
Throughout this article, we have explored the multifaceted nature of dry eye disease, from its symptoms and causes to effective diagnostic techniques and treatment options. It’s common to feel overwhelmed by environmental influences, such as low humidity and prolonged screen time, alongside systemic factors like hormonal changes and medication side effects, which can exacerbate this condition. Comprehensive assessment methods, including patient history and specific ocular tests, ensure accurate diagnosis, while tailored management strategies—ranging from artificial tears to advanced therapies—offer relief and improved eye health.
The significance of understanding and addressing dry eye disease cannot be overstated. As awareness grows and new research emerges, we encourage individuals to seek guidance from healthcare professionals to explore the most suitable treatment options. By prioritizing eye care and making informed lifestyle adjustments, it is possible to alleviate symptoms and enhance overall well-being. Taking these steps not only empowers you in your eye health journey but also contributes to a broader understanding of this common yet often overlooked condition.
Frequently Asked Questions
What is dry eye disease?
Dry eye disease occurs when the eyes do not produce enough moisture or when the fluid evaporates too quickly, leading to discomfort.
What are the common symptoms of dry eye disease?
Common symptoms include persistent dryness, burning or stinging sensations, redness, sensitivity to light, and blurred vision that often improves with blinking.
What causes dry eye disease?
The causes of dry eye disease include tear film instability, chronic inflammation of the ocular surface, and meibomian gland dysfunction, which decreases oil production and increases moisture evaporation.
How does tear film instability affect dry eye disease?
Tear film instability disrupts the lubrication of the eye, which can lead to inadequate moisture and exacerbate symptoms of dry eye disease.
What role does meibomian gland dysfunction play in dry eye disease?
Meibomian gland dysfunction decreases oil production in the tears, resulting in increased evaporation of moisture, which contributes to the symptoms of dry eye disease.