Posted by: Northwest Eye in General on August 3, 2025
Overview
This article addresses the essential steps for supportive therapy in managing subconjunctival hemorrhage, focusing on reassurance and relief from discomfort. We understand that experiencing this condition can be concerning, but it’s important to note that it is typically harmless and often resolves on its own. Supportive measures, such as:
- Applying cold compresses
- Using artificial tears
can help alleviate discomfort during this time.
It’s common to feel anxious about your symptoms, and we want to reassure you that seeking medical attention is crucial if your symptoms worsen or persist beyond two weeks. Remember, you are not alone in this process—we are here to help you through it. Taking proactive steps can make a difference in your comfort and recovery.
Introduction
Subconjunctival hemorrhage, often presenting as a striking red patch on the eye, can understandably raise alarm for those who encounter it. While this condition is typically harmless, it can arise from various causes, such as:
- Sudden pressure changes
- The use of blood-thinning medications
Understanding the supportive therapy options available not only alleviates discomfort but also empowers you to manage your eye health effectively. We understand that facing persistent symptoms or complications can be concerning. Exploring the essential steps for care can provide clarity and reassurance as you navigate this common ocular occurrence.
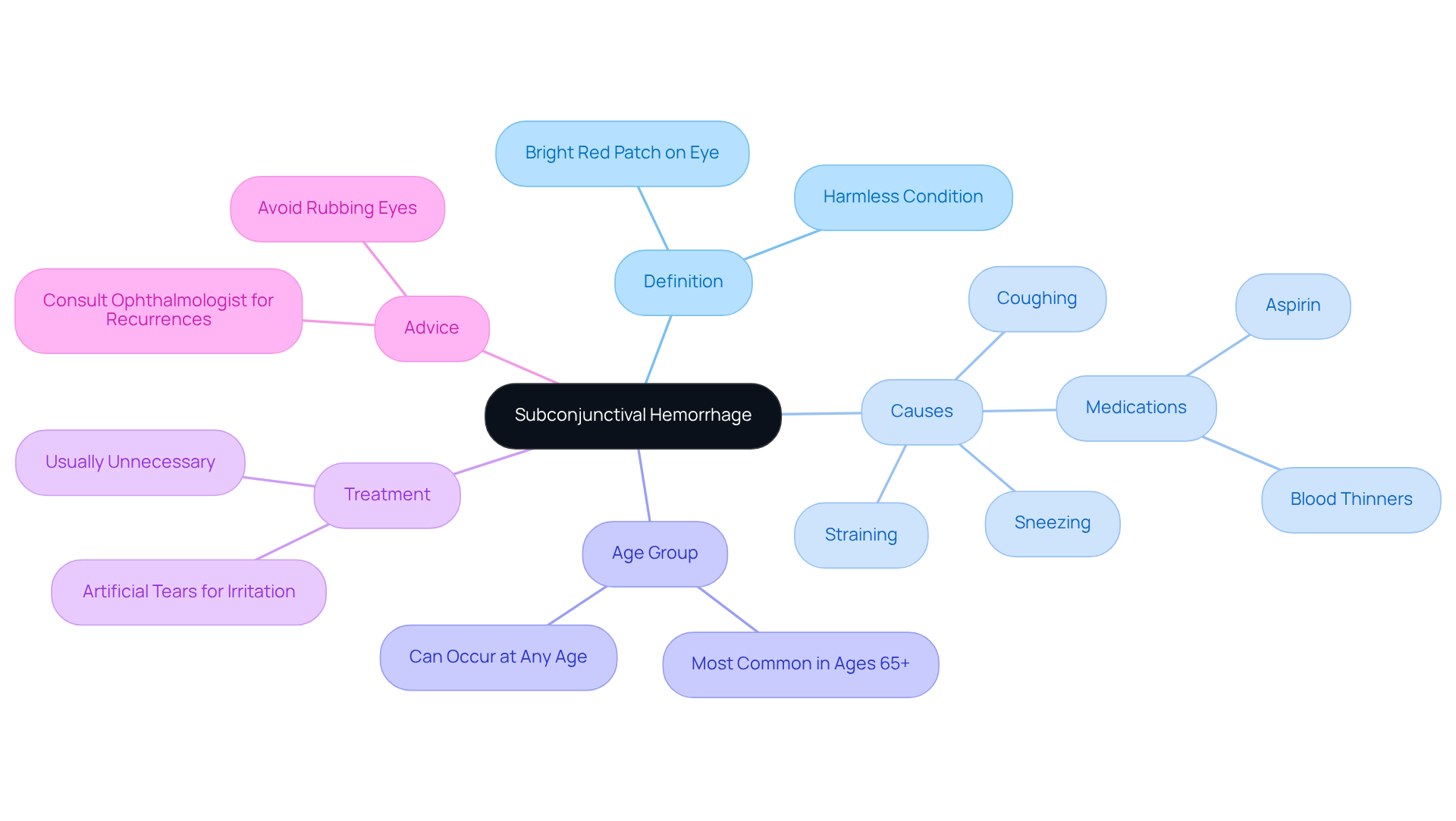
Understand Subconjunctival Hemorrhage: Definition and Overview
Subconjunctival bleeding can be concerning when you notice a bright red patch on the white part of your eye. This happens when a small vessel ruptures beneath the conjunctiva, the transparent membrane that covers the sclera. While it may look alarming, we want you to know that this condition is typically harmless. Think of it like a bruise on your skin; just as a bruise heals, the fluid from this bleeding is usually reabsorbed by your body within one to two weeks.
It’s common to feel worried about what might have caused this bleeding. It can occur due to actions that elevate pressure in the veins, such as:
- Coughing
- Sneezing
- Straining
Additionally, certain medications, like aspirin and blood thinners, can contribute to this condition. While subconjunctival bleeding is most frequently seen in individuals aged 65 and older, it can happen to adults of any age, often without a clear reason. In fact, about 10% of people may experience it again without identifiable risk factors.
Understanding this condition, along with subconjunctival hemorrhage supportive therapy, can help demystify the appearance of your eye and reassure you that it is often benign. Most cases resolve on their own, and subconjunctival hemorrhage supportive therapy is rarely necessary. However, if you experience mild irritation, artificial tears can provide relief. If you find that you have frequent occurrences, we encourage you to consult an ophthalmologist for further evaluation. As the bleeding subsides, it’s normal for the white of your eye to appear yellowish during the healing process. Remember, we are here to help you through this experience and answer any questions you may have.
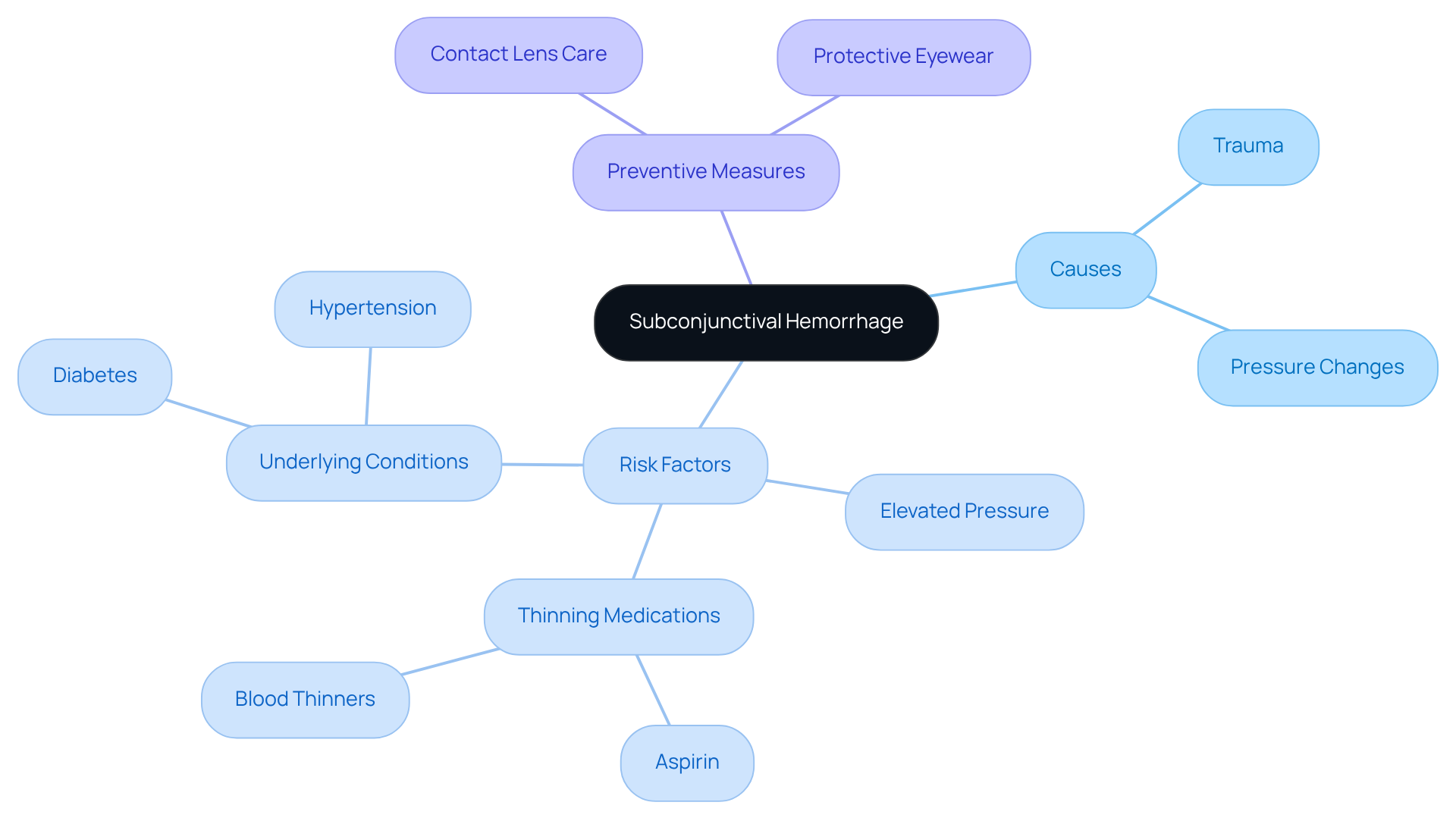
Identify Causes and Risk Factors of Subconjunctival Hemorrhage
Subconjunctival hemorrhage can arise from various causes, and we understand that this can be concerning. It primarily involves trauma to the eye, such as rubbing or injury. Additionally, sudden rises in pressure from actions like coughing, sneezing, or straining can lead to the rupture of small vessels in the conjunctiva.
Key risk factors include:
- Elevated pressure in the circulatory system
- The use of thinning medications like aspirin
- Underlying health conditions such as diabetes
It’s important to note that individuals taking anticoagulants may experience a greater frequency of recurrence for eye bleeding. Understanding these triggers is crucial for you to identify potential risks in your daily activities and implement preventive measures.
For example, maintaining the cleanliness of contact lenses and using suitable protective eyewear during sports and activities can greatly lower the chances of encountering eye bleeding. Furthermore, recurrent episodes, particularly in children and the elderly, can signify systemic conditions like hypertension or diabetes, which may warrant further evaluation by an eye care professional.
Most instances of eye bleeding are not severe and usually clear up independently within a few weeks, with most injured vessels recovering within two weeks. Remember, we are here to help you through this process and provide support as you navigate your health.
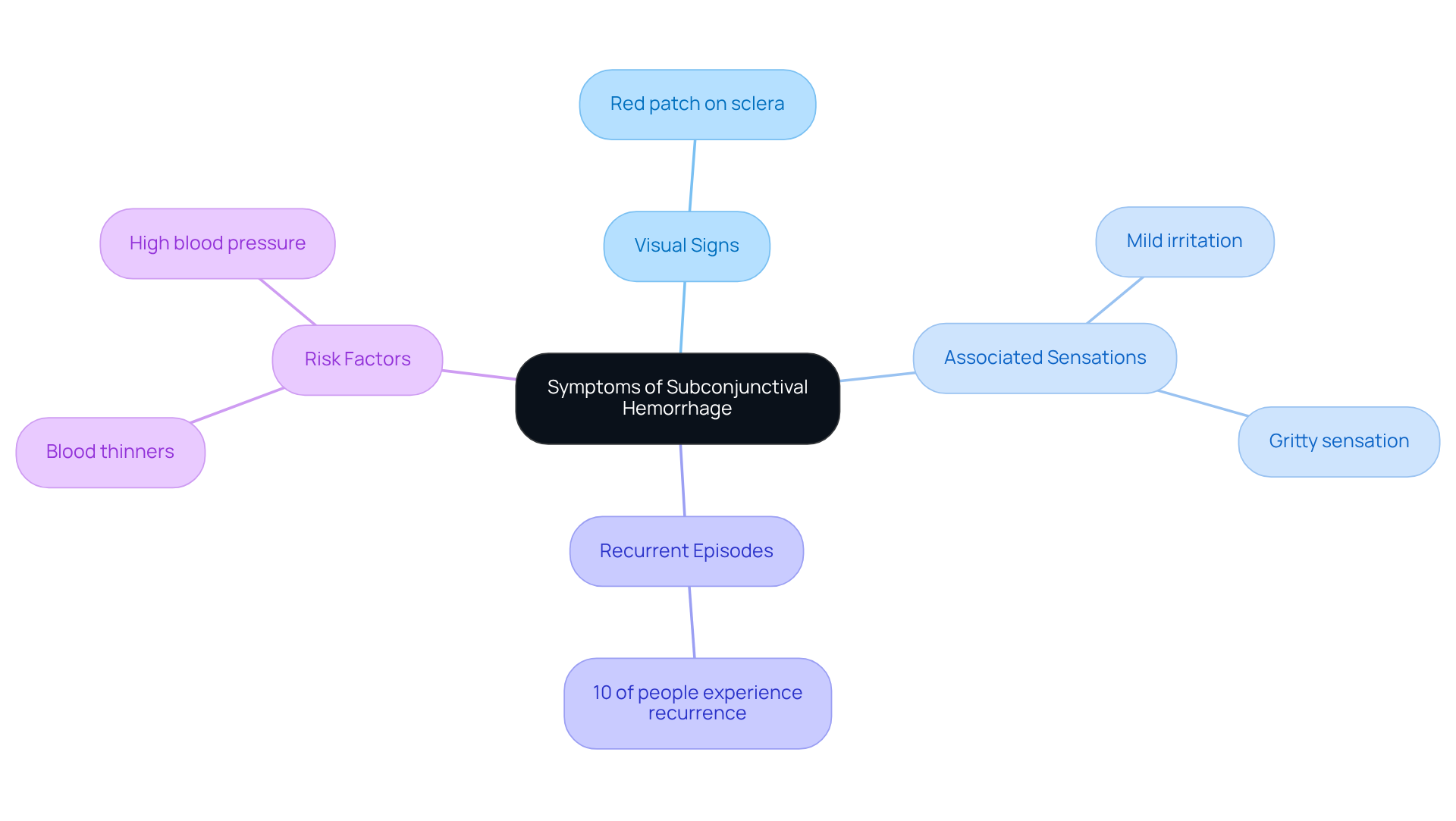
Recognize Symptoms of Subconjunctival Hemorrhage
A red patch on the sclera, or the white part of your eye, can be a vivid sign of bleeding beneath the conjunctiva. We understand that seeing this noticeable discoloration might be alarming. Typically, it does not come with pain, swelling, or changes in vision, which helps distinguish it from more serious eye conditions. While the appearance may be startling, most individuals report only mild irritation or a gritty sensation. In fact, about 10% of people may experience recurrent episodes, often linked to underlying risk factors such as blood thinners or high blood pressure.
Identifying these signs is essential, as it can provide comfort. Despite its concerning appearance, eye bleeding is usually harmless and resolves on its own within two weeks. If irritation persists or if you notice additional symptoms, such as eye pain, we encourage you to consult a healthcare provider. These could indicate more serious conditions that require further evaluation. Remember, we are here to help you through this process and ensure your well-being.
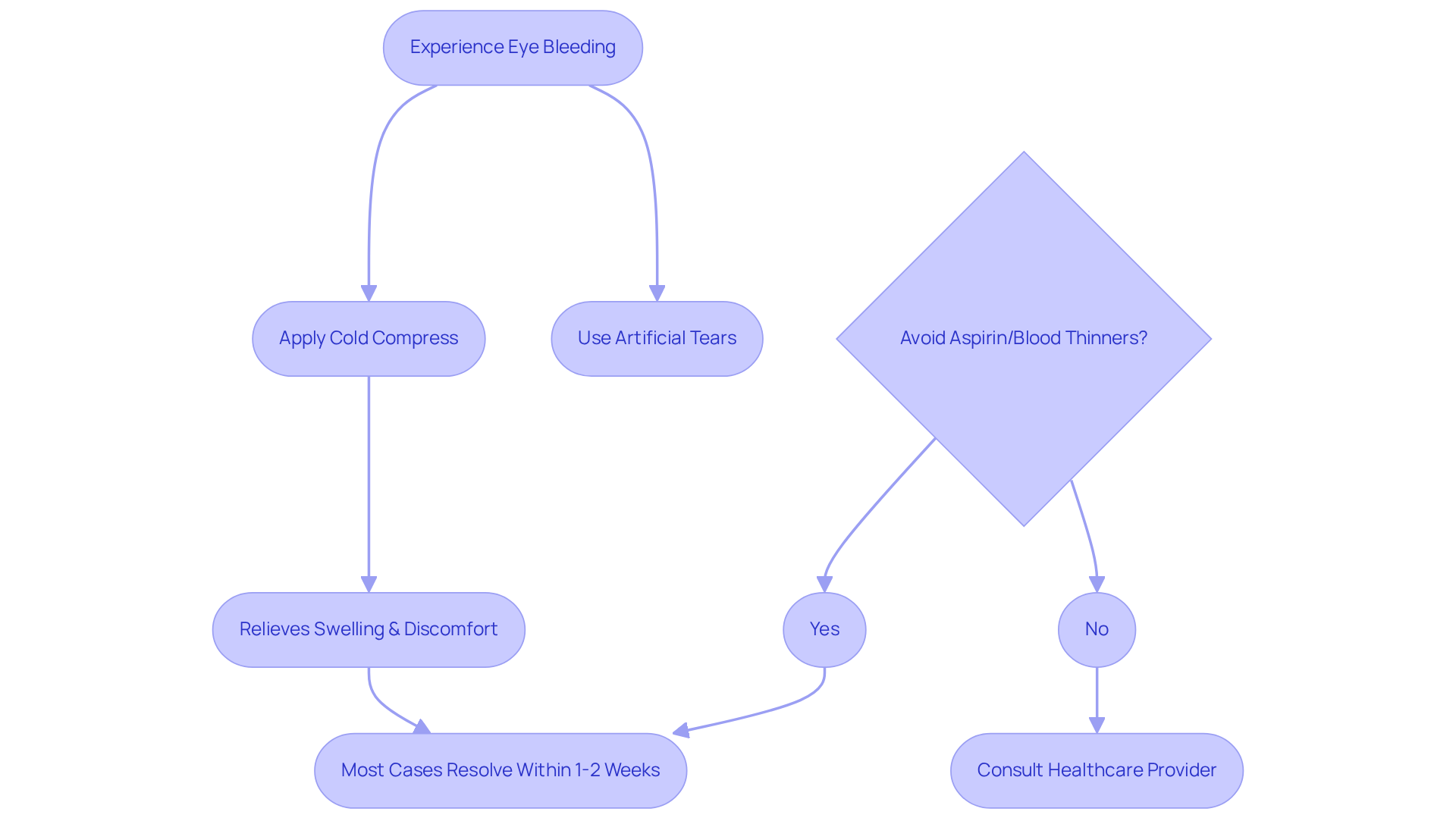
Implement Supportive Therapy for Subconjunctival Hemorrhage Management
Subconjunctival hemorrhage supportive therapy for managing eye bleeding focuses on reassurance and symptom relief. We understand that experiencing eye bleeding can be concerning. Applying cold compresses to the affected eye can significantly reduce swelling and discomfort, especially in the initial days following the incident. This method is particularly effective as it helps constrict blood vessels and minimize inflammation. Additionally, using artificial tears can alleviate any scratchy sensations, providing further comfort during the healing process.
It’s crucial to avoid aspirin or other blood-thinning medications unless specifically prescribed by a healthcare provider, as these can exacerbate bleeding. While most cases resolve on their own within one to two weeks, it’s common to feel anxious about the possibility of recurrence. About 10% of individuals without known risk factors may experience a recurrence of eye bleeding. If bleeding persists beyond two weeks, we encourage you to consult with an eye care professional to rule out any serious underlying conditions.
Older individuals might face an increased risk for eye bleeding due to reduced elasticity in connective tissue. While subconjunctival hemorrhage supportive therapy can enhance comfort, it’s reassuring to know that most eye bleeding episodes resolve on their own, reinforcing the benign nature of the condition. Remember, we are here to help you through this process.
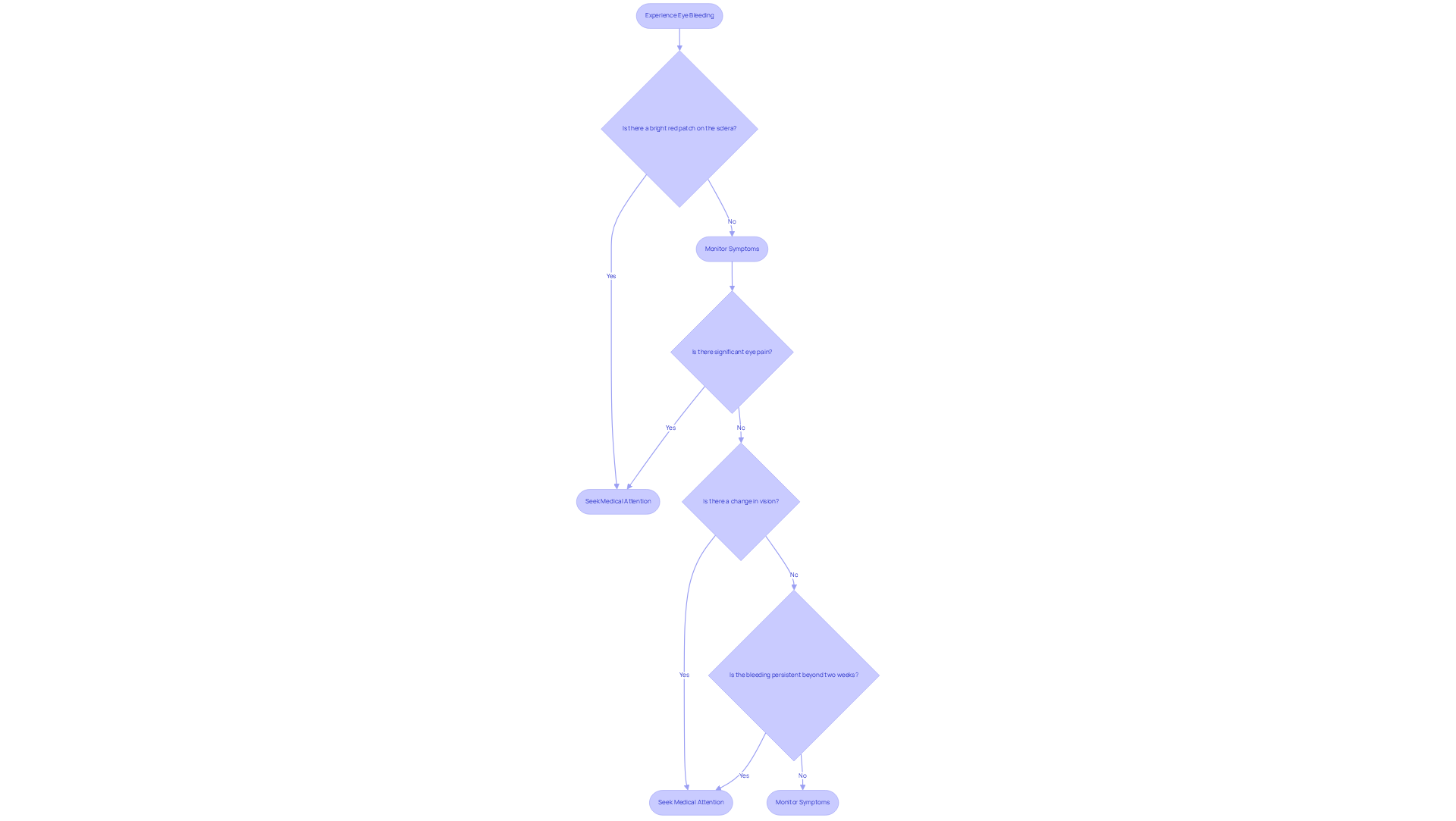
Determine When to Seek Medical Attention
While eye bleeding is often harmless, it’s important to recognize specific warning signs that indicate the need for swift medical assessment. One of the most noticeable signs is a bright red patch on the sclera, or the white part of the eye. If you experience significant eye pain, changes in vision, or if the bleeding persists beyond two weeks without improvement, we encourage you to seek prompt attention.
Additionally, signs of infection, such as pus or increased redness around the eye, warrant urgent consultation with a healthcare provider. It’s common to feel anxious about these symptoms, but addressing them quickly can help ensure your well-being. Persistent high blood pressure can also increase the risk of eye bleeding, highlighting the importance of effectively managing your health conditions.
Recognizing these critical symptoms is essential for ensuring timely intervention and minimizing the risk of complications. Untreated subconjunctival hemorrhages, for instance, can lead to more serious conditions, including retinal detachment or infections, especially if accompanied by trauma or ongoing bleeding. Supportive measures, like ice packs and artificial tears, can provide comfort during your recovery when combined with subconjunctival hemorrhage supportive therapy.
Understanding these indicators empowers you to take proactive steps in managing your eye health effectively. Remember, we are here to help you through this process, and your health is our priority.
Conclusion
Subconjunctival hemorrhage, while visually alarming, is typically a benign condition that can often resolve on its own. We understand that this eye condition may cause anxiety, and recognizing that the bright red patch on the sclera is akin to a bruise and usually harmless can help you approach the situation with greater confidence and clarity.
Throughout this guide, we’ve shared key insights regarding the causes, symptoms, and supportive therapies for subconjunctival hemorrhage. From identifying risk factors such as high blood pressure and the use of blood thinners to implementing simple home care techniques like cold compresses and artificial tears, our aim is to empower you in your self-care journey. It’s common to feel uncertain, but knowing when to seek medical attention—such as in cases of persistent bleeding or significant discomfort—ensures that any potential complications are addressed promptly.
Ultimately, maintaining awareness of subconjunctival hemorrhage and its management is essential for your eye health. By taking proactive steps and seeking support when necessary, you can navigate this condition with ease and reassurance. Remember, being informed is key to managing your health effectively—don’t hesitate to reach out to a healthcare provider if concerns arise. We are here to help you through this process.
Frequently Asked Questions
What is subconjunctival hemorrhage?
Subconjunctival hemorrhage is a condition where a small vessel ruptures beneath the conjunctiva, causing a bright red patch on the white part of the eye. It is typically harmless and resembles a bruise on the skin.
What causes subconjunctival hemorrhage?
It can occur due to actions that elevate pressure in the veins, such as coughing, sneezing, or straining. Trauma to the eye, like rubbing or injury, can also lead to this condition.
Who is most likely to experience subconjunctival hemorrhage?
While it is most frequently seen in individuals aged 65 and older, it can occur in adults of any age, often without a clear reason. About 10% of people may experience it again without identifiable risk factors.
How long does it take for subconjunctival hemorrhage to heal?
The bleeding usually resolves on its own within one to two weeks as the fluid is reabsorbed by the body.
Are there any risk factors associated with subconjunctival hemorrhage?
Key risk factors include elevated pressure in the circulatory system, the use of thinning medications like aspirin, and underlying health conditions such as diabetes. Individuals taking anticoagulants may experience more frequent recurrences.
What should I do if I experience mild irritation from subconjunctival hemorrhage?
If you experience mild irritation, using artificial tears can provide relief.
When should I consult an ophthalmologist regarding subconjunctival hemorrhage?
If you have frequent occurrences of subconjunctival hemorrhage, it is advisable to consult an ophthalmologist for further evaluation.
What changes might I notice in the appearance of my eye during the healing process?
As the bleeding subsides, it is normal for the white of your eye to appear yellowish during the healing process.
What preventive measures can I take to reduce the risk of subconjunctival hemorrhage?
Preventive measures include maintaining the cleanliness of contact lenses, using suitable protective eyewear during sports and activities, and being cautious to avoid actions that elevate pressure in the veins.