Posted by: Northwest Eye in General on August 21, 2025
Overview
Enucleation of the eye is a surgical procedure that may feel daunting, but it is primarily indicated for conditions such as:
- Intraocular tumors
- Severe trauma
- Painful blind eyes
- Unresponsive infections
Our goal is to preserve your overall health and alleviate any discomfort you may be experiencing. We understand that considering such a procedure can bring up many emotions, and it’s important to know that enucleation is often only considered after all other treatment options have been exhausted.
In this article, we will detail the procedure, recovery process, and potential risks involved. It’s common to feel apprehensive about surgery, but we are here to help you through this process, providing the information you need to feel supported and informed. Remember, you are not alone in this journey; many patients have faced similar challenges and found reassurance in understanding their options.
We encourage you to reach out with any questions or concerns. Your well-being is our priority, and we are committed to supporting you every step of the way.
Introduction
Deciding to undergo an enucleation, the complete removal of an eye, can be a profound and unsettling experience. It’s often a choice made in response to serious medical conditions such as intraocular tumors, severe trauma, or persistent pain from a blind eye. We understand that this surgical procedure, while necessary for preserving your overall health, raises critical questions about the process, recovery, and potential risks involved.
How can you best prepare for this life-altering surgery? What steps can you take to ensure a smoother recovery while navigating the emotional and physical challenges that may arise? This article delves into the enucleation procedure, offering a comprehensive overview of what to expect before, during, and after the surgery. We will also discuss the risks and management strategies that can help facilitate your healing and adaptation. Remember, we are here to help you through this process.
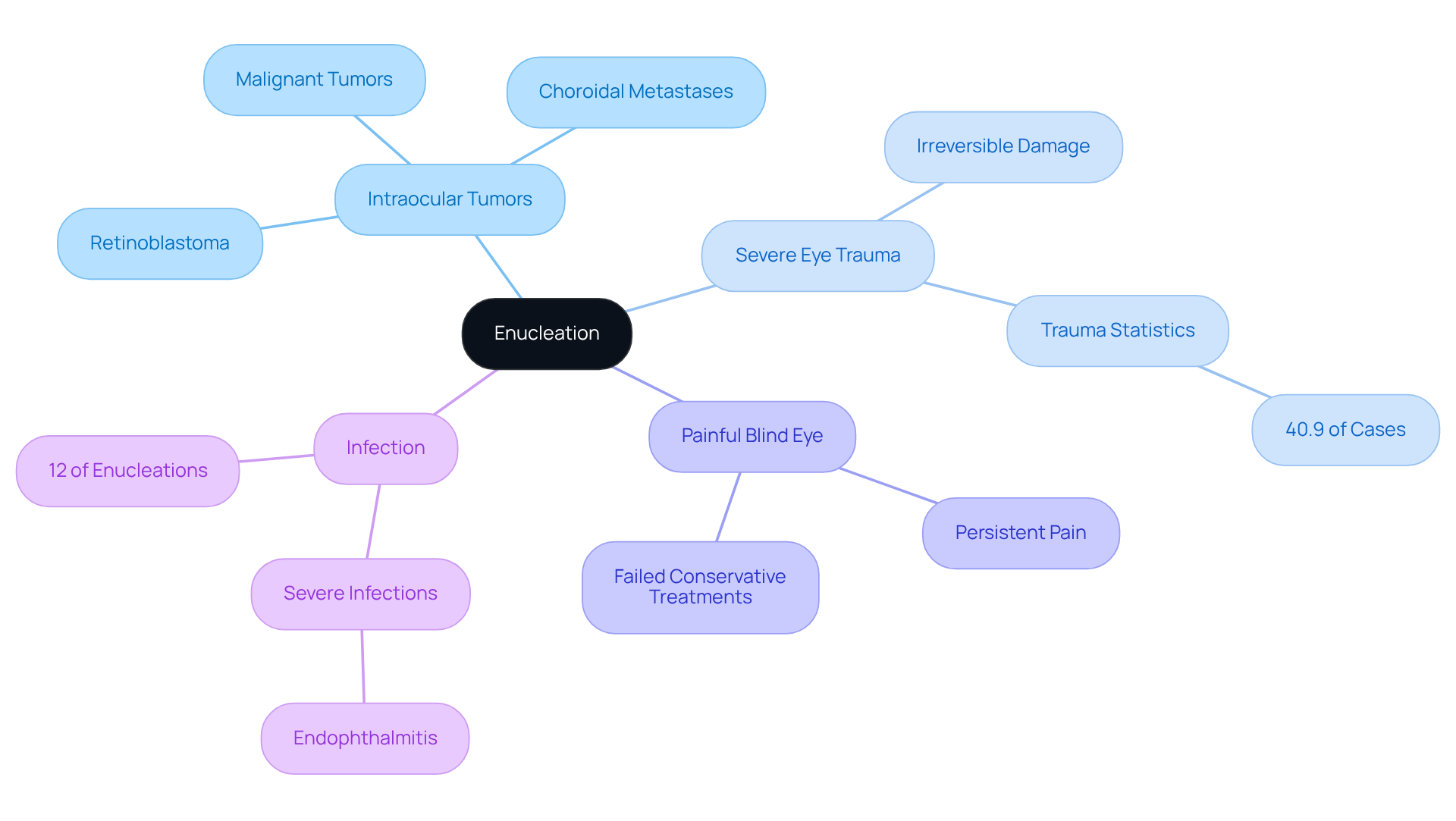
Define Enucleation: Purpose and Indications
The enucleation of eye is a surgical procedure that involves the complete removal of the eyeball (globe) from its socket, while carefully preserving the surrounding tissues and muscles. We understand that facing such a procedure can be daunting, and it’s important to know that this intervention is primarily indicated for several critical conditions:
- Intraocular Tumors: Enucleation is often performed to address malignant tumors, such as retinoblastoma and uveal melanoma, where the tumor poses a significant risk of metastasis. Recent studies indicate that choroidal metastases, frequently originating from breast and lung cancers, are the most common intraocular tumors in adults. This procedure is necessary to prevent further complications and ensure your well-being.
- In cases of severe eye trauma, where the eye experiences irreversible harm, enucleation of eye may be necessary to relieve pain and prevent additional health complications. It’s important to note that trauma accounts for about 40.9% of cases involving eye removal in the U.S., particularly among children, where penetrating injuries or serious accidents are common.
- Painful Blind Eye: If you or a loved one is dealing with a blind eye that leads to persistent pain or discomfort, considering the enucleation of eye may improve quality of life. This decision is often made when conservative treatments fail to provide relief, and we are here to support you through this process.
- In situations where an eye infection does not respond to treatment and poses a risk to overall health, an enucleation of eye may be required to eradicate the source of infection. This is particularly relevant in severe infections like endophthalmitis, which can lead to significant complications if not addressed promptly.
Understanding these indications empowers you and your family to make and available treatment options. As noted by ophthalmologists, ‘Enucleation of eye is typically the last careful arrangement that an ophthalmologist arrives at when all the helpful alternatives for a given determination have been considered previously.’ Furthermore, it is essential to acknowledge that retinoblastoma is the leading reason for the enucleation of eye in the first three years of life, emphasizing the importance of this procedure in pediatric situations. We are here to help you through this journey, ensuring you receive the support you need.
Describe the Enucleation Procedure: Step-by-Step Overview
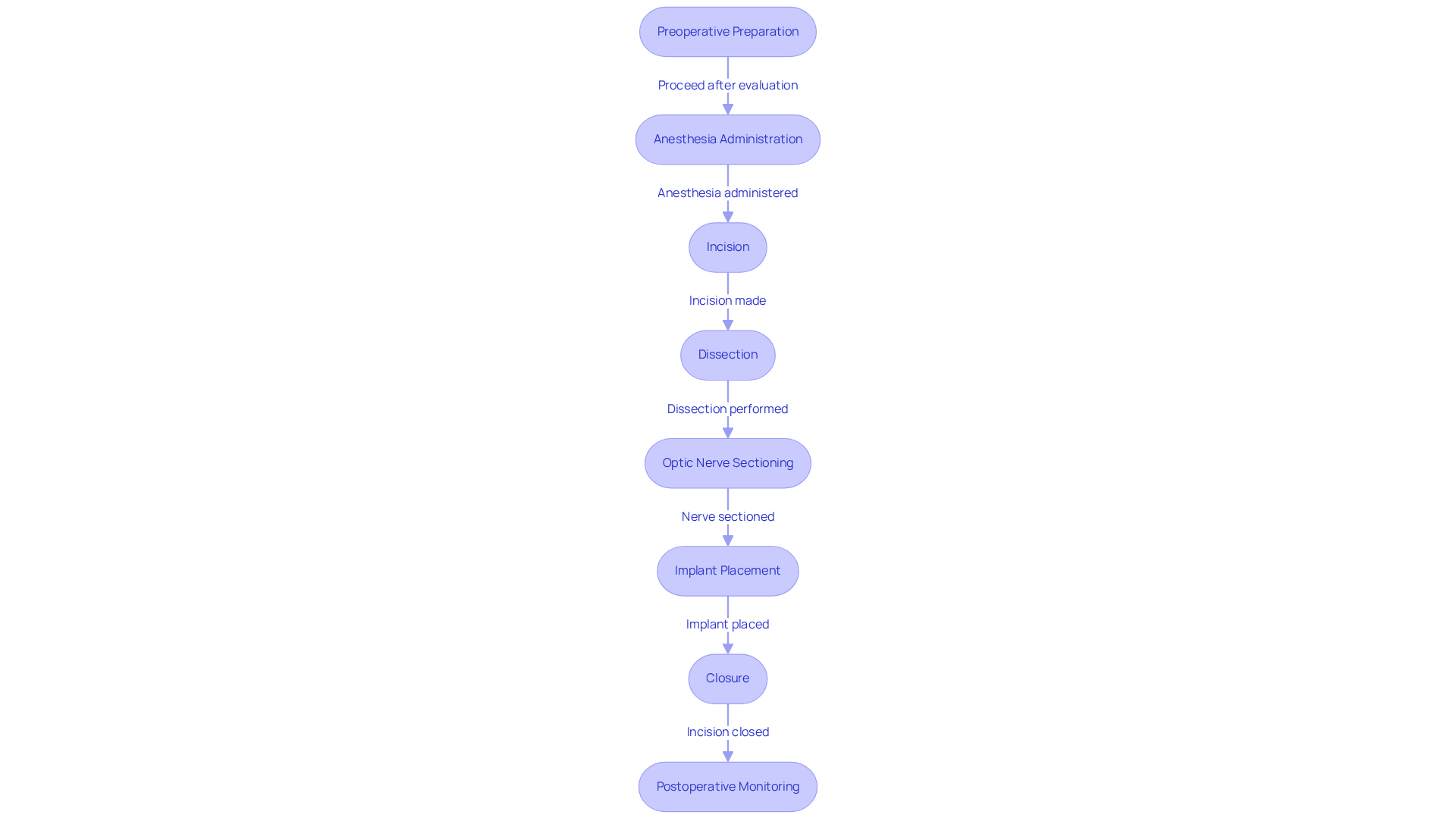
The enucleation procedure typically follows these steps:
- Preoperative Preparation: We understand that preparing for surgery can be daunting. Patients undergo a thorough evaluation to identify any medical conditions that may impact the surgery. During this phase, anesthesia options are reviewed, ensuring that individuals are well-informed and prepared for the procedure. As noted by SickKids staff, “Before any procedure, it is important to talk honestly with your child about what will happen and to use language that they will understand.”
- Anesthesia Administration: It’s common to feel anxious about anesthesia. To ensure comfort for the individual, general anesthesia is administered. This method enables a during the surgery, with the anesthesiologist closely observing the individual’s vital signs. An ocularist emphasizes, “It is important to remain very still when the impression is being made as this will ensure the best fit of your artificial eye.”
- Incision: A conjunctival peritomy is performed, creating an incision around the eye to access the underlying tissues. This step is crucial for providing the necessary access to the eye and surrounding structures.
- Dissection: The Tenon capsule is carefully separated from the sclera, and the eye muscles are meticulously dissected to free the eye from its attachments. This precision is vital to avoid damage to surrounding tissues.
- Optic Nerve Sectioning: The optic nerve is clamped and cut, facilitating the complete removal of the eye. This step is essential for ensuring that all connections are severed, allowing for a clean extraction.
- Implant Placement: Following the removal of the eye, a spherical implant is placed in the orbit to maintain the shape of the eye socket. This implant is designed to support the eyelids and provide a foundation for a future prosthetic eye.
- Closure: The incision is closed with sutures, and a conformer is placed to support the eyelids during the healing process. This helps to ensure proper alignment and reduces the risk of complications.
- Postoperative Monitoring: After the procedure, patients are closely observed for any immediate complications before being transferred to the recuperation area. This monitoring is essential for detecting any problems early and ensuring a smooth restoration.
Recent advancements in cell removal methods have centered on reducing trauma and enhancing recovery durations. Surgeons now utilize enhanced imaging technologies and refined surgical instruments, which contribute to better outcomes and reduced postoperative complications. For example, the surgical procedure usually takes between 1 to 2 hours, and individuals may remain in the hospital for approximately two days after the operation. Real-life experiences from individuals emphasize the significance of comprehensive preoperative conversations about anesthesia choices, as many convey relief at having a clear understanding of what to anticipate during the procedure. Overall, this organized method guarantees that the procedure is conducted securely and efficiently, fostering ideal healing and patient contentment.
Outline Post-Operative Care: Recovery and Management
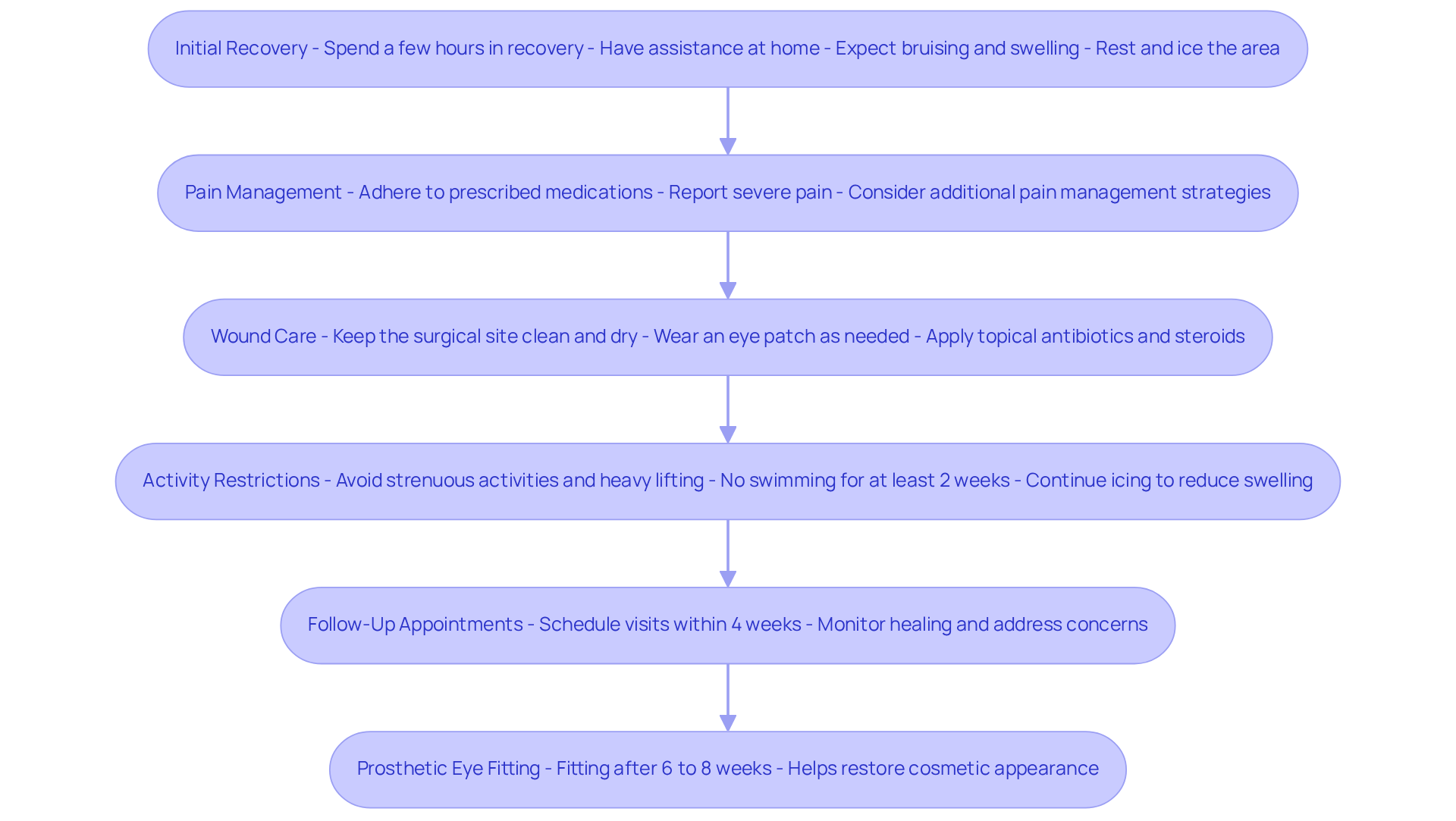
Post-operative care after the enucleation of the eye is essential for a successful healing process. We understand that this can be a challenging time, and we are here to help you through it. Here are key aspects to consider:
- Initial Recovery: Patients typically spend a few hours in recovery before being discharged. It’s advisable to have someone assist you at home during the initial days. Expect some bruising and swelling, similar to what you might experience with blepharoplasty healing, and plan to rest at home for a few days. Frequent icing applied to the area can help reduce swelling, as recommended for blepharoplasty recovery.
- Pain Management: Effective pain relief is crucial. You will be prescribed medications to manage discomfort, and it’s important to adhere to the prescribed dosage. We emphasize that reporting any severe pain is vital for timely intervention. Research suggests that many individuals express a wish for after surgery, highlighting the necessity for efficient pain control protocols. For instance, half of those experiencing persistent postsurgical pain (PPSP) report at least mild to severe discomfort, underscoring the significance of proactive pain management.
- Wound Care: Keeping the surgical site clean and dry is paramount. You may need to wear an eye patch for a specified period to protect the area and promote healing. Additionally, the application of topical antibiotics and steroids is recommended for up to 30 days after surgery to assist in healing. Proper wound care can significantly reduce the risk of complications.
- Activity Restrictions: To prevent complications, it’s important to avoid strenuous activities, heavy lifting, and swimming for at least two weeks following surgery. This period is critical for allowing the surgical site to heal properly. Frequent icing can also help reduce swelling during this time.
- Follow-Up Appointments: Regular follow-up visits are essential to monitor healing and address any concerns. Please arrange these meetings as instructed by your surgeon, usually within four weeks after surgery, to ensure a smooth healing process.
- Prosthetic Eye Fitting: After a healing period of 6 to 8 weeks, you can be fitted for a prosthetic eye, which can help restore your cosmetic appearance. This fitting is a crucial phase in the healing process, as it aids in adapting to life following the enucleation of the eye.
By following these recommendations, you will promote a more seamless healing process and assist yourself in adapting to life after removal. Practical examples indicate that individuals who adhere to these suggestions frequently express greater contentment with their healing journey.
Identify Risks and Complications: What to Watch For
While the is generally a safe procedure, we understand that patients may have concerns about potential risks and complications during recovery. It’s important to stay vigilant and informed:
- Infection: Signs of infection can manifest as increased redness, swelling, or discharge from the surgical site. If you notice these symptoms, please reach out to your healthcare provider. Research shows that post-operative infections occur in about 10% of cases involving enucleation of eye, highlighting the importance of monitoring for these signs.
- Bleeding: Some bleeding is expected, but if you experience excessive bleeding or notice blood clots, it’s crucial to report this to your physician immediately. While post-operative hemorrhage is uncommon, it can occur, especially in individuals on blood thinners.
- Scarring: Scarring at the incision site may impact your cosmetic appearance. We encourage you to discuss any concerns regarding scarring with your surgeon to explore potential interventions that can help.
- Eyelid Issues: Complications such as drooping eyelids (ptosis) or difficulty fully closing the eyelids may arise. These issues can be addressed with further surgical intervention if needed.
- Implant Complications: Complications related to the orbital implant, such as extrusion or exposure, may require additional surgical procedures. Research indicates that approximately 21.7% of individuals experience implant complications after the enucleation of eye.
- Psychological Impact: The emotional and psychological effects of losing an eye can be significant. We encourage you to seek support from mental health professionals to navigate these challenges effectively.
By being aware of these risks and monitoring for concerning symptoms, you can facilitate a smoother recovery. Remember, we are here to help you through this process and address any complications promptly.

Conclusion
The enucleation of the eye is a critical surgical procedure aimed at alleviating severe medical conditions, including intraocular tumors, traumatic injuries, and painful blind eyes. We understand that facing such a decision can be daunting, and this intervention highlights the importance of timely and informed decision-making regarding eye health. It provides relief in situations where other treatments have failed. By understanding the rationale behind enucleation, patients and their families can navigate this challenging experience with greater confidence and support.
Throughout this article, we outline key aspects of the enucleation procedure, from preoperative preparation and the surgical steps to post-operative care and potential risks. Emphasis is placed on the significance of effective pain management, proper wound care, and regular follow-up appointments to ensure a smooth recovery. It’s common to feel anxious about possible complications, such as infection and psychological impacts, and being aware of these can foster a proactive approach to healing.
Ultimately, the enucleation of the eye serves not only as a medical necessity but also as a pivotal moment in a patient’s journey towards improved quality of life. By remaining informed and vigilant about the procedure and its aftermath, individuals can enhance their recovery experience. Seeking support and guidance is essential, as the emotional and physical challenges of this surgery can be significant. Embracing this journey with knowledge and care can lead to a more positive outcome, paving the way for adaptation and healing in the wake of such a profound change.
Frequently Asked Questions
What is enucleation?
Enucleation is a surgical procedure that involves the complete removal of the eyeball (globe) from its socket while preserving the surrounding tissues and muscles.
What are the main indications for enucleation?
Enucleation is primarily indicated for several critical conditions, including intraocular tumors, severe eye trauma, painful blind eye, and eye infections that do not respond to treatment.
Why is enucleation performed for intraocular tumors?
Enucleation is performed to address malignant tumors, such as retinoblastoma and uveal melanoma, that pose a significant risk of metastasis and to prevent further complications.
How common is eye removal due to trauma?
Trauma accounts for about 40.9% of cases involving eye removal in the U.S., particularly among children, often due to penetrating injuries or serious accidents.
When is enucleation considered for a painful blind eye?
Enucleation may be considered when a blind eye causes persistent pain or discomfort and conservative treatments fail to provide relief, potentially improving the patient’s quality of life.
In what cases might enucleation be necessary due to infections?
Enucleation may be required for severe eye infections, such as endophthalmitis, that do not respond to treatment and pose a risk to overall health.
How do ophthalmologists view enucleation in the context of treatment options?
Ophthalmologists typically consider enucleation as a last resort after all other treatment options for a given condition have been evaluated.
What is the leading reason for enucleation in young children?
Retinoblastoma is the leading reason for enucleation of the eye in the first three years of life, highlighting the importance of this procedure in pediatric cases.