Posted by: Northwest Eye in Glaucoma on October 20, 2025
Overview
Primary open-angle glaucoma (POAG) is a common eye condition that many may not be aware of. It is characterized by a gradual increase in intraocular pressure, which can lead to optic nerve damage. Often, this occurs without early symptoms, making regular eye exams crucial for detection and management. We understand that this can be concerning, and we want to assure you that you are not alone in this journey.
The article highlights several risk factors, including:
- Age
- Family history
- Ethnicity
- Elevated intraocular pressure
It’s important to be aware of these factors as they can help guide your care. Treatments for POAG are available, including:
- Medications
- Laser therapy
- Surgery
These options are designed to manage the condition effectively and prevent vision loss, providing you with the reassurance you need.
We are here to help you through this process, ensuring that you receive the support and care necessary for your eye health. Remember, taking action by scheduling regular eye exams is a vital step in safeguarding your vision.
Introduction
Understanding primary open-angle glaucoma is crucial, as it silently threatens the vision of millions without warning. We recognize how alarming this can be. Often referred to as the ‘sneak thief of sight,’ this condition gradually increases intraocular pressure, which can lead to potential optic nerve damage. In this article, we will explore the risks, symptoms, and treatment options available to you, emphasizing the importance of early detection and proactive management. It’s common to feel uncertain about your eye health, but we are here to help you safeguard your vision against this insidious disease.
Define Primary Open-Angle Glaucoma
Primary open angle glaucoma is the most common type of primary open angle glaucoma, and it can be concerning to learn about it. This condition is characterized by a gradual rise in intraocular pressure (IOP) as the eye’s drainage canals become less effective over time. Unlike angle-closure eye conditions, the drainage angle remains open, but the fluid does not drain effectively, which can lead to optic nerve damage.
It’s important to note that this condition is often asymptomatic in its early stages, earning it the nickname ‘the sneak thief of sight.’ Approximately 95% of individuals with this eye condition are affected by primary open angle glaucoma, which typically impacts both eyes. However, one eye may be more severely impacted than the other. Early detection is critical to prevent irreversible vision loss, and we understand how vital it is for individuals, especially those over 40 years of age, to be aware of this condition.
Current statistics indicate that over 4 million Americans are living with this eye condition, with more than 2 million aged 40 and older specifically affected by primary open angle glaucoma. Research suggests that up to half of individuals with the eye condition may be unaware they have it, particularly in the over-40 age group. Regular eye exams, including dilated eye assessments, are essential for early detection and management, helping to preserve vision and enhance quality of life.
As Dr. Lisa M. Young, OD, FAAO, emphasizes, ‘Regular eye exams not only keep your vision sharp but also detect signs of systemic health conditions like diabetes and high blood pressure.’ Furthermore, this eye condition imposes a significant economic burden, costing the U.S. economy approximately $2.86 billion annually in direct costs and productivity losses.
We are here to help you through this process, and we encourage you to prioritize your eye health by scheduling regular check-ups. Remember, taking action now can make a difference in your vision and overall well-being.
Identify Risk Factors for POAG
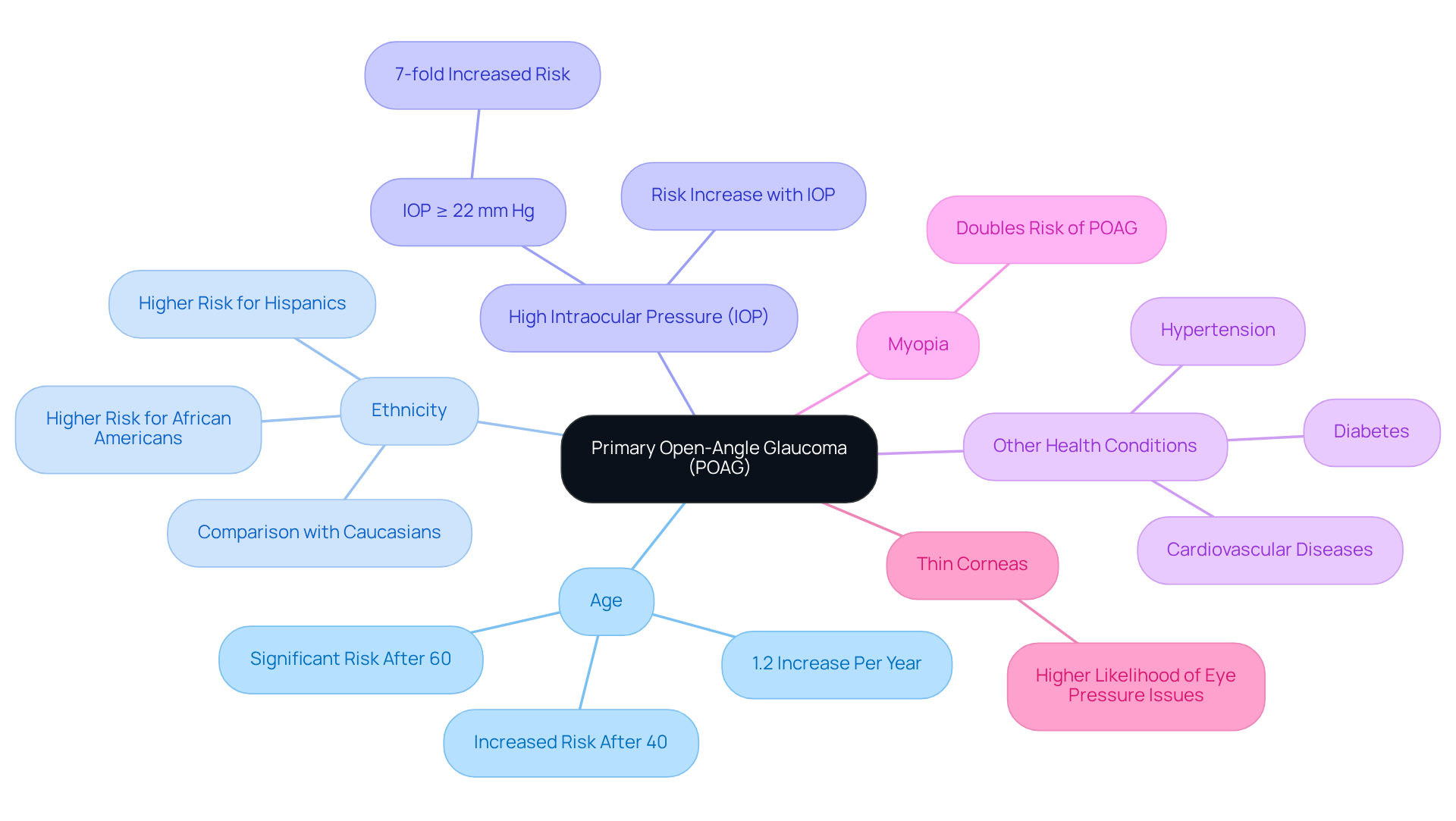
Primary Open-Angle Glaucoma (POAG) is influenced by several key risk factors that we want you to be aware of:
- Age: We understand that as individuals grow older, the risk of developing POAG escalates significantly, especially for those over 40. After age 60, this risk becomes even more pronounced. Research indicates that for every extra year of age, the likelihood of developing eye disease increases by about 1.2%. Family history is significant because if glaucoma runs in your family, it can increase your chances of developing primary open-angle glaucoma by as much as 2.85 times. This highlights the significance of genetic predisposition in evaluating your vulnerability.
- Ethnicity: Certain ethnic groups, particularly African Americans and Hispanics, face a greater likelihood of developing POAG compared to Caucasians. This calls for targeted awareness and screening efforts tailored to these communities.
- High Intraocular Pressure (IOP): Elevated IOP is a primary threat factor for POAG. If your IOP levels are 22 mm Hg or higher, you have a seven-fold heightened chance of developing primary open angle glaucoma.
- Other Health Conditions: We recognize that comorbidities such as diabetes, hypertension, and cardiovascular diseases can further increase the likelihood of elevated intraocular pressure. This underscores the necessity for comprehensive health management.
- Myopia: If you are nearsighted, it’s worth noting that there is an association with an increased chance of POAG. Evidence suggests that myopia may double the likelihood of developing this condition.
- Thin Corneas: A reduced central corneal thickness is linked to a higher likelihood of eye pressure issues. This makes regular eye examinations essential for early detection and peace of mind.
Understanding these risk factors is essential for proactive management and early intervention in glaucoma care. We are here to help you through this process, ensuring you have the support and information you need.
Recognize Symptoms of POAG
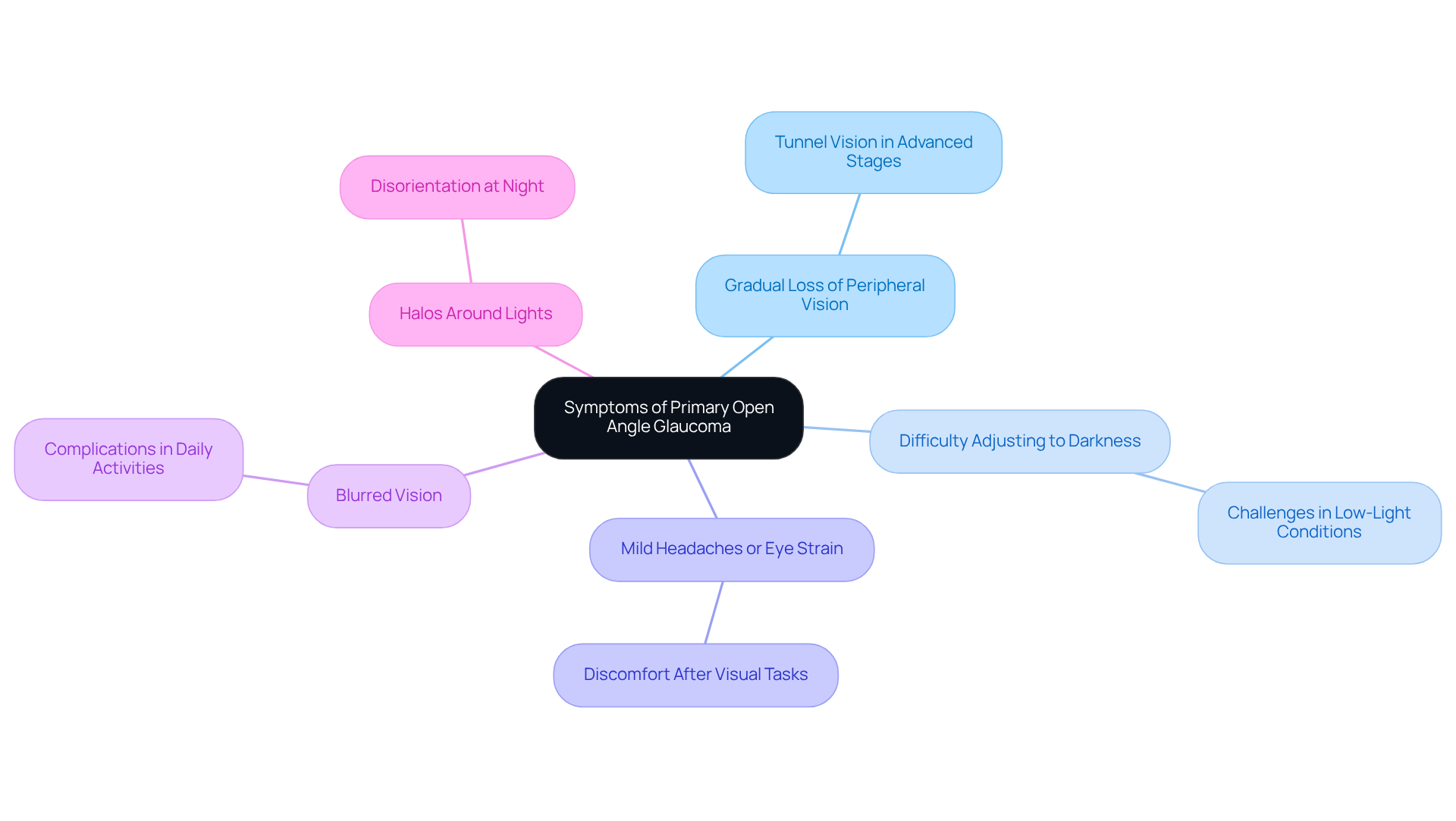
Primary open angle glaucoma is commonly known as the ‘sneak thief of sight,’ and this is justified as it often remains unnoticed during its early stages. We understand that this can be concerning, especially as the condition progresses and symptoms begin to emerge. Here are some key signs to watch for:
- Gradual Loss of Peripheral Vision: This is typically the first noticeable sign, leading to what many describe as ‘tunnel vision’ in advanced stages. It can feel alarming as your field of vision narrows, making it challenging to see objects to the side.
- Difficulty Adjusting to Darkness: You may find it increasingly hard to see in low-light conditions, impacting your ability to navigate in dimly lit environments.
- Mild Headaches or Eye Strain: It’s common to experience discomfort, especially after extended periods of visual tasks. This can often be mistaken for simple fatigue.
- Blurred Vision: As the optic nerve sustains damage, blurred vision may occur, complicating daily activities and adding to your worries.
- Halos Around Lights: Many patients notice halos around bright lights, particularly at night, which can be disorienting and unsettling.
Due to the subtlety of these symptoms, we encourage you to prioritize regular eye exams for early detection and management of primary open angle glaucoma. Many patients have shared their experiences, expressing that they initially dismissed these symptoms as normal aging or fatigue. Recognizing these signs early can lead to timely intervention, potentially preserving vision and improving your quality of life. Remember, we are here to help you through this process, providing support and guidance every step of the way.
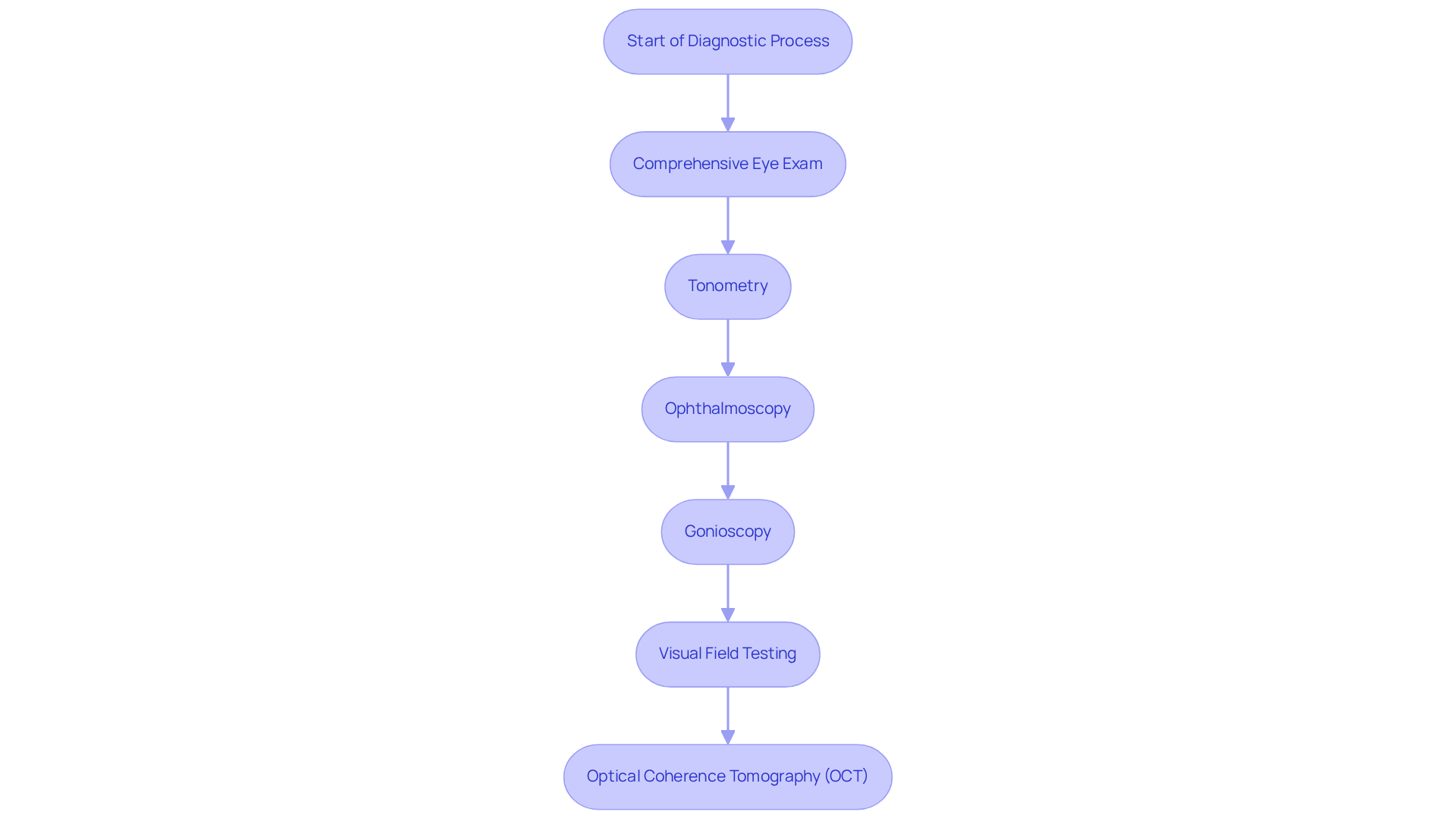
Understand the Diagnostic Process for POAG
We understand that facing the diagnostic process for primary open angle glaucoma can be daunting. It typically involves several key assessments that are crucial for your eye health and peace of mind:
- Comprehensive Eye Exam: This includes a detailed medical history and visual acuity tests to ensure we understand your vision needs.
- Tonometry: This test measures intraocular pressure (IOP) to determine if it is elevated, which is an important indicator of glaucoma.
- Ophthalmoscopy: An examination of the optic nerve helps us check for any damage or changes that may suggest increased intraocular pressure.
- Gonioscopy: This test evaluates the drainage angle of your eye, confirming that it is open and functioning properly.
- Visual Field Testing: This assesses your peripheral vision, helping us identify any loss that may indicate glaucoma.
- Optical Coherence Tomography (OCT): This imaging test provides detailed images of the optic nerve and retinal layers, aiding in the early detection of any damage.
We are here to support you through this process. These assessments are not just tests; they are essential steps in establishing a diagnosis for primary open angle glaucoma and determining the best treatment plan tailored to your needs. Remember, you are not alone in this journey, and we are committed to providing the care and reassurance you deserve.
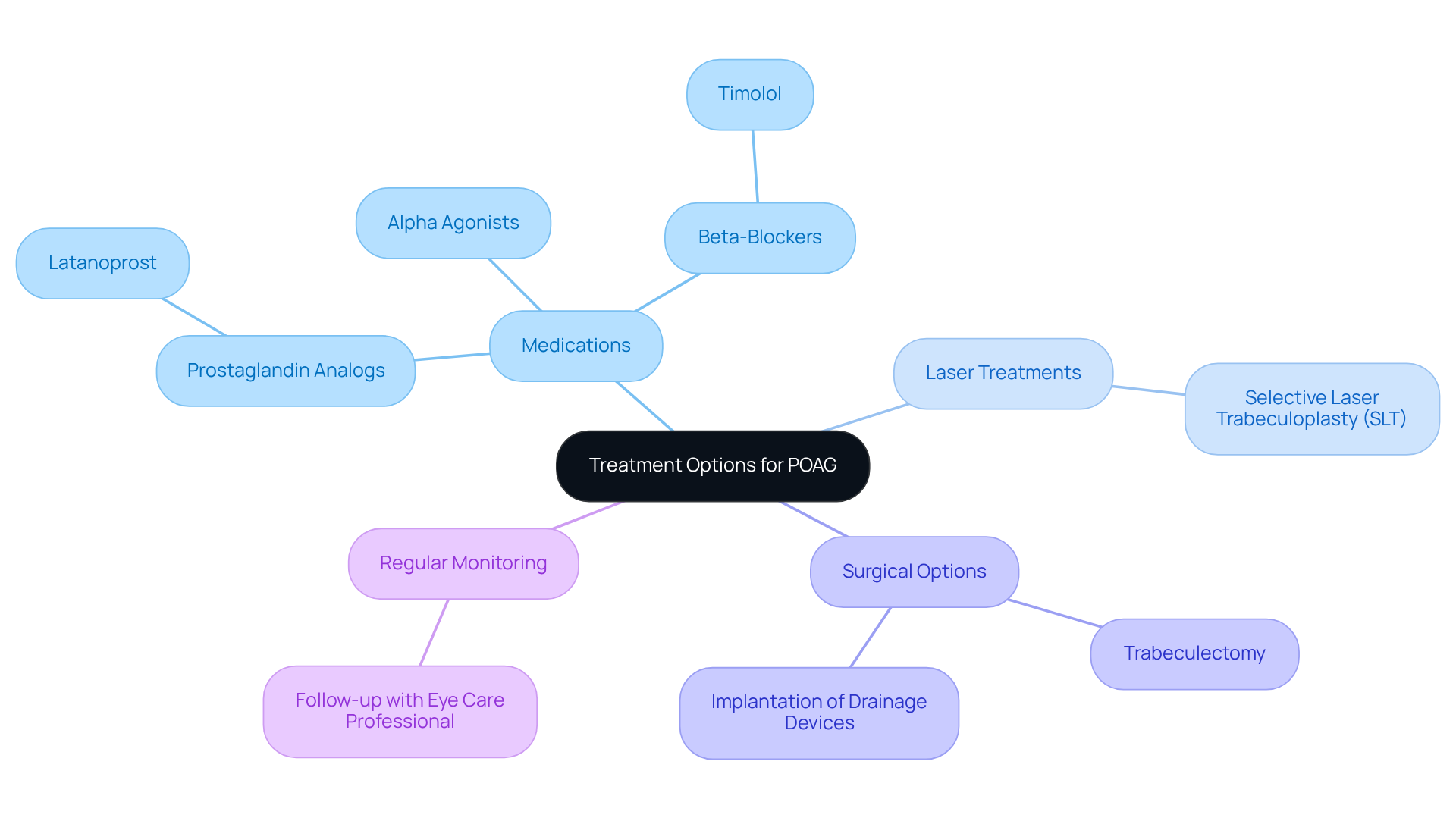
Explore Treatment Options for POAG
Treatment for primary open angle glaucoma is focused on lowering intraocular pressure (IOP) and preventing further damage to the optic nerve. We understand that navigating primary open angle glaucoma can be overwhelming, but there are several options available to help you manage it effectively.
-
Medications: Typically, the first line of treatment involves prescription eye drops that help reduce IOP. Common classes include:
- Prostaglandin Analogs: Such as latanoprost, which work by increasing fluid drainage.
- Beta-Blockers: Such as timolol, which help decrease fluid production.
- Alpha Agonists: These also contribute to reducing fluid production and enhancing drainage.
-
Laser Treatments: Procedures like selective laser trabeculoplasty (SLT) can significantly improve drainage and lower IOP.
-
Surgical Options: In cases where medications and laser treatments may not be sufficient, surgical interventions such as trabeculectomy or the implantation of drainage devices may be necessary.
-
Regular Monitoring: Continuous follow-up with your eye care professional is essential. This allows for the assessment of treatment effectiveness and necessary adjustments over time.
We encourage you to work closely with your ophthalmologist to determine the best treatment plan tailored to your specific needs. Remember, you are not alone in this journey; we are here to help you through the process and ensure you receive the care you deserve.
Conclusion
Primary open-angle glaucoma (POAG) is a significant health concern that can progress quietly, yet it carries the potential for severe vision loss. We understand how daunting this condition can be, especially for individuals over the age of 40. Early detection and intervention are crucial, as they can greatly influence outcomes. The gradual rise in intraocular pressure, coupled with the absence of noticeable symptoms in the early stages, makes it vital to stay aware and have regular eye examinations to preserve your vision.
This article highlights several key aspects of POAG, including its:
- Definition
- Risk factors
- Symptoms
- Diagnostic processes
- Treatment options
Recognizing that age, ethnicity, and family history can increase risk is essential. Additionally, subtle symptoms such as gradual peripheral vision loss and difficulty adjusting to darkness are important to note. These insights emphasize the importance of proactive eye care. The diagnostic process, which includes comprehensive eye exams and various tests, is crucial for timely intervention.
Treatment options, ranging from medications to surgical interventions, provide effective pathways to manage this condition. We are here to help you navigate these choices and ensure you receive the care you need.
Ultimately, prioritizing your eye health through regular check-ups and staying informed about the risks and symptoms of primary open-angle glaucoma can empower you to take control of your vision. As the saying goes, “an ounce of prevention is worth a pound of cure.” By remaining vigilant and proactive, you can confidently navigate the complexities of POAG, ensuring that you maintain your quality of life and vision for years to come.
Frequently Asked Questions
What is primary open-angle glaucoma (POAG)?
Primary open-angle glaucoma is the most common type of glaucoma, characterized by a gradual rise in intraocular pressure (IOP) due to ineffective drainage of fluid in the eye. This condition can lead to optic nerve damage and is often asymptomatic in its early stages.
Who is most affected by primary open-angle glaucoma?
Approximately 95% of individuals with glaucoma are affected by primary open-angle glaucoma, which typically impacts both eyes, although one eye may be more severely affected. Over 4 million Americans have this condition, with more than 2 million aged 40 and older.
Why is early detection of POAG important?
Early detection of primary open-angle glaucoma is critical to prevent irreversible vision loss. Many individuals, especially those over 40, may be unaware they have the condition, making regular eye exams essential for management and preservation of vision.
What are the key risk factors for developing primary open-angle glaucoma?
Key risk factors for POAG include age (risk increases significantly after age 40), family history of glaucoma, ethnicity (higher risk in African Americans and Hispanics), high intraocular pressure (IOP of 22 mm Hg or higher), other health conditions (such as diabetes and hypertension), myopia (nearsightedness), and thin corneas.
How does age influence the risk of POAG?
The risk of developing primary open-angle glaucoma escalates significantly with age, particularly for individuals over 40, and increases even more after age 60. Research shows that for each additional year of age, the likelihood of developing eye disease increases by about 1.2%.
What is the economic impact of primary open-angle glaucoma in the U.S.?
Primary open-angle glaucoma imposes a significant economic burden on the U.S. economy, costing approximately $2.86 billion annually in direct costs and productivity losses.
How can individuals manage their risk for POAG?
Individuals can manage their risk for primary open-angle glaucoma by scheduling regular eye exams, being aware of their family history, maintaining overall health, and monitoring for other risk factors such as elevated intraocular pressure and comorbidities.