Posted by: Northwest Eye in General on October 29, 2025
Overview
Eye transplant surgery is a hopeful option for those seeking to restore their vision through procedures such as corneal transplants. We understand that the journey can be daunting, as it comes with challenges like:
- Rejection risks
- Surgical complications
- Limited donor tissue availability
It’s common to feel anxious about these issues, and we want to acknowledge your concerns.
As we explore this topic, it’s important to highlight the future innovations that may bring comfort and reassurance. Advancements such as:
- Stem cell therapy
- Improved surgical techniques
are on the horizon, promising to enhance success rates and accessibility for patients like you. We are here to help you through this process, offering support every step of the way.
Your feelings are valid, and we recognize the importance of addressing them. By staying informed and hopeful, you can take proactive steps towards your vision restoration journey.
Introduction
Eye transplant surgery represents a beacon of hope for individuals grappling with vision loss. We understand that this journey can be daunting, filled with both promise and challenges. This article delves into the various types of eye transplant procedures, from the more common corneal transplants to the experimental whole eye transplants. We will highlight the critical steps involved in the surgical process, ensuring you feel informed and supported.
However, it’s common to feel apprehensive about the potential for rejection, limited donor availability, and the emotional toll of surgery. Many may wonder:
- What does the future hold for eye transplantation?
- How can emerging innovations reshape the landscape of ocular health?
We are here to help you through this process, providing insights and encouragement as you navigate this complex field.
Explore the Fundamentals of Eye Transplant Surgery
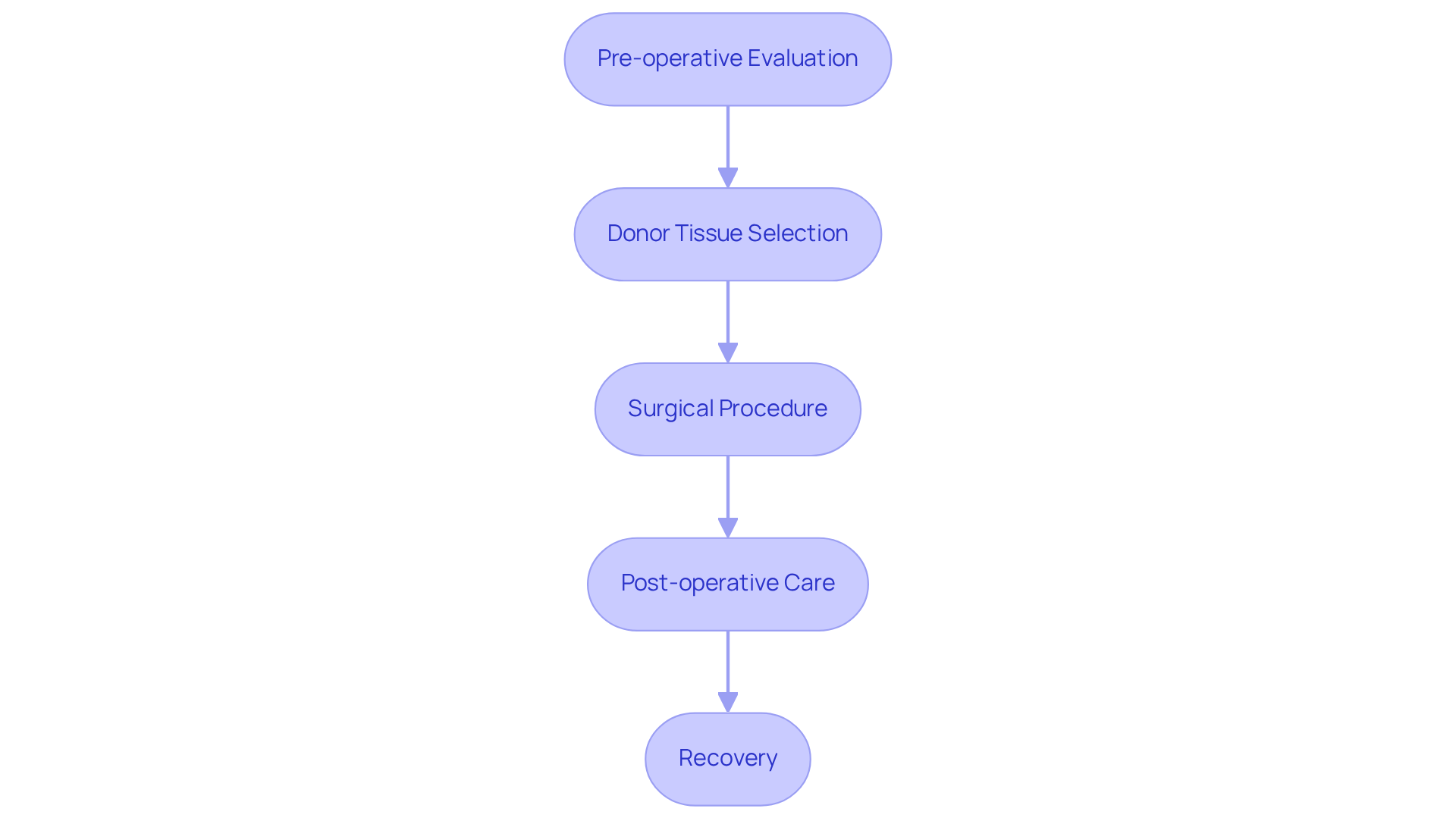
Eye transplant surgery consists of specialized operations aimed at restoring vision by replacing damaged or diseased eye tissues, particularly through corneal transplants. We understand that considering such a procedure can bring about many emotions, and it’s important to feel informed and supported throughout this journey. The process involves several critical steps:
-
Pre-operative Evaluation: A comprehensive examination is conducted to assess your eye health and determine your suitability for transplantation. This assessment is essential, as it helps identify any underlying conditions that may influence the procedure’s success. It’s common to feel apprehensive, but rest assured that this evaluation is a vital step in ensuring optimal conditions for your operation. You may need to discontinue specific medications, such as aspirin and ibuprofen, 7 to 10 days prior to the procedure.
-
Donor Tissue Selection: Surgeons carefully select donor tissues that meet stringent compatibility criteria. This selection process is crucial to minimize the risk of rejection, ensuring the best possible outcome for you.
-
Surgical Procedure: The operation is performed under anesthesia, either general or local, based on your needs. During eye transplant surgery, the damaged cornea is meticulously removed and replaced with healthy donor tissue, which is essential for restoring your vision.
-
Post-operative Care: After the procedure, you will receive detailed recovery instructions, including the use of prescribed medications to prevent infection and manage inflammation. A follow-up appointment is necessary the day after the corneal surgery to monitor your healing and address any complications that may arise.
Statistics indicate that corneal procedures are the most prevalent form of organ replacement in the U.S., with over 137,000 tissue recoveries recorded in 2023 alone. Many individuals experience notable vision enhancement within weeks, while others may require up to a year for complete recovery. We hope this information helps you understand the intricacies of eye replacement procedures and their impact on your care and recovery.
Differentiate Between Corneal and Whole Eye Transplants
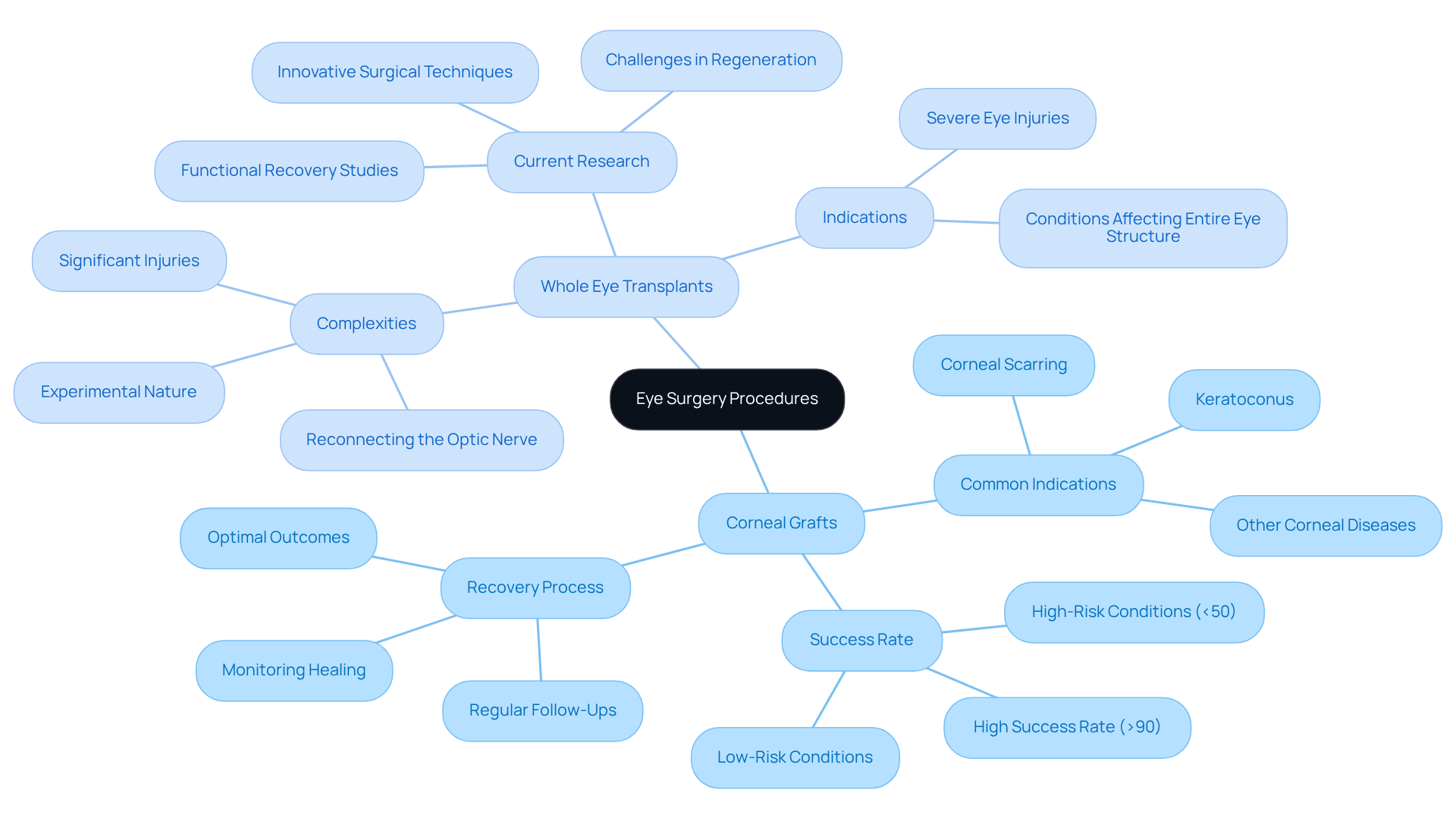
Eye surgery procedures can be categorized into two main types: corneal operations and whole eye procedures.
-
Corneal Grafts: This is the most common type of eye procedure, involving the replacement of the cornea, the clear front part of the eye. We understand that considering surgery can be daunting, but it’s important to know that common indications for corneal surgeries include corneal scarring, keratoconus, and other corneal diseases. The success rate for these surgeries is notably high, often exceeding 90% in low-risk conditions. Recovery typically involves regular follow-ups to monitor healing and ensure optimal outcomes, providing peace of mind during your journey to better vision.
-
Whole eye transplants are a type of eye transplant surgery that involves the transplantation of the entire eye and are considerably rarer. We recognize that this may sound complex, and it’s essential to understand that complete eye transplant surgery remains primarily experimental. These surgeries are usually considered for individuals with significant injuries or conditions affecting the entire eye structure. The complexities of this surgery include the intricate challenge of reconnecting the optic nerve, which is essential for restoring vision. Current research is focused on overcoming these challenges, with ongoing studies exploring innovative surgical techniques and the potential for functional recovery.
Grasping these differences is essential for both patients and healthcare professionals as they explore treatment choices. We are here to help you through this process, ensuring that you feel supported and informed about the consequences of each type of procedure.
Identify Challenges and Limitations in Eye Transplantation
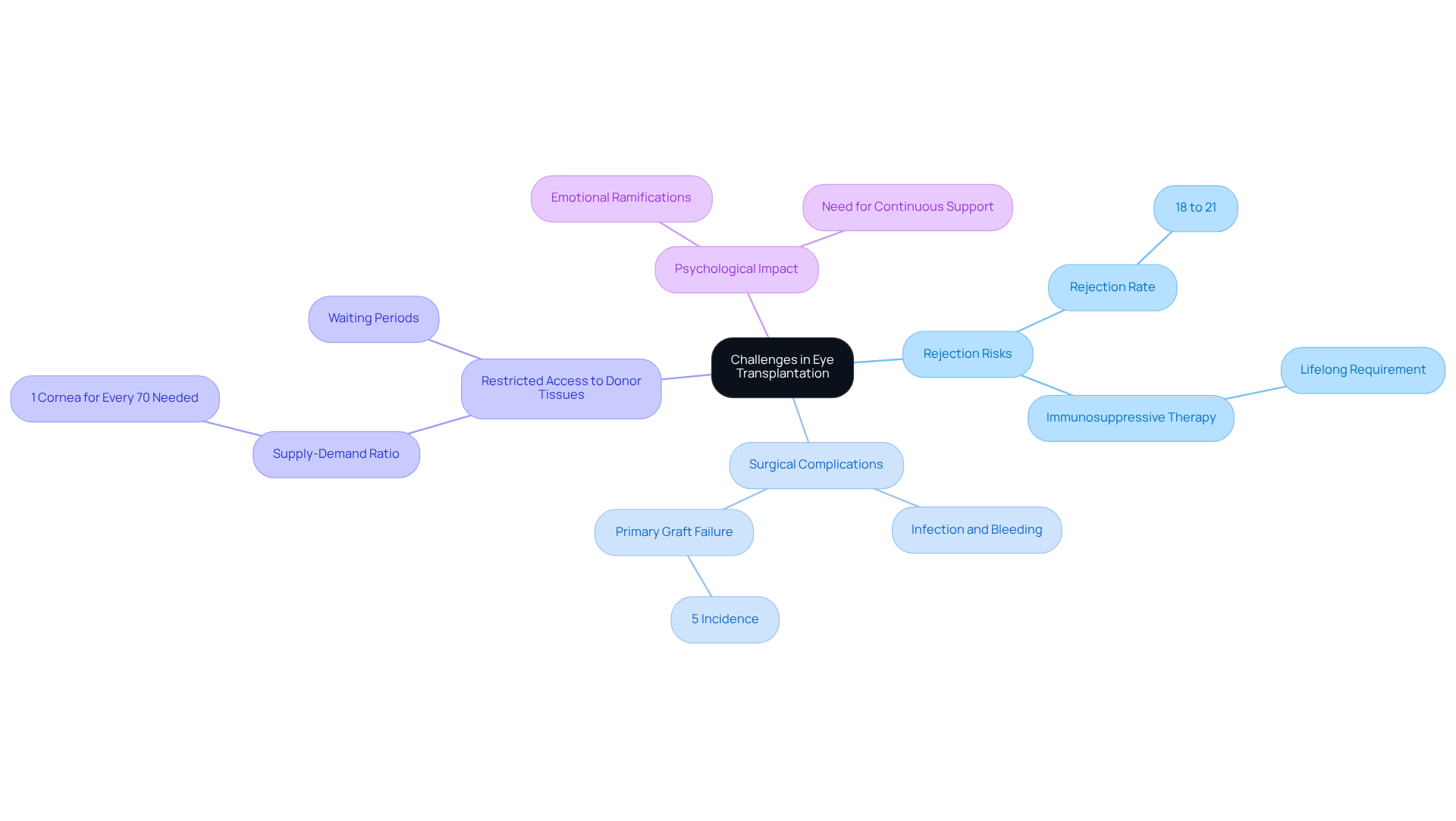
Eye transplantation offers hope for restoring vision, but it also presents several significant challenges and limitations that we understand can be concerning:
-
Rejection Risks: It’s important to know that, like other organ procedures, eye surgeries carry the risk of rejection. This occurs when the recipient’s immune system targets the donor tissue. To help prevent rejection episodes, which can occur in approximately 18% to 21% of cases, lifelong immunosuppressive therapy is necessary. For corneal graft recipients, the likelihood of rejection falls within this range, and we recognize how daunting this can feel.
-
Surgical Complications: Potential complications from eye surgery, such as infection, bleeding, and healing difficulties, can significantly impact the success of the procedure. Studies indicate that the average incidence of primary graft failure in Descemet stripping endothelial keratoplasty (DSEK) can be as high as 5%. We understand that these statistics may raise questions and concerns about the surgery.
-
Restricted Access to Donor Tissues: The need for donor tissues often exceeds the available supply, leading to prolonged waiting periods for those in need. With only one cornea available for every 70 needed worldwide, the gap between supply and demand is stark. It’s common to feel anxious about the waiting process, and we are here to support you through it.
-
Psychological Impact: Undergoing such a significant procedure can have profound emotional and psychological ramifications. Many patients find they need continuous assistance and guidance to navigate the complexities of their condition and the outcomes of the procedure. We want you to know that you are not alone in this journey.
Addressing these challenges is crucial for enhancing patient outcomes and improving the overall success rates of eye transplant surgery. Ongoing research, including collaboration with over 40 experts in the Transplantation of Human Eye Allografts (THEA) program, aims to tackle these issues and improve future transplantation efforts. We are here to help you through this process and provide the support you need.
Anticipate Future Innovations in Eye Transplant Surgery
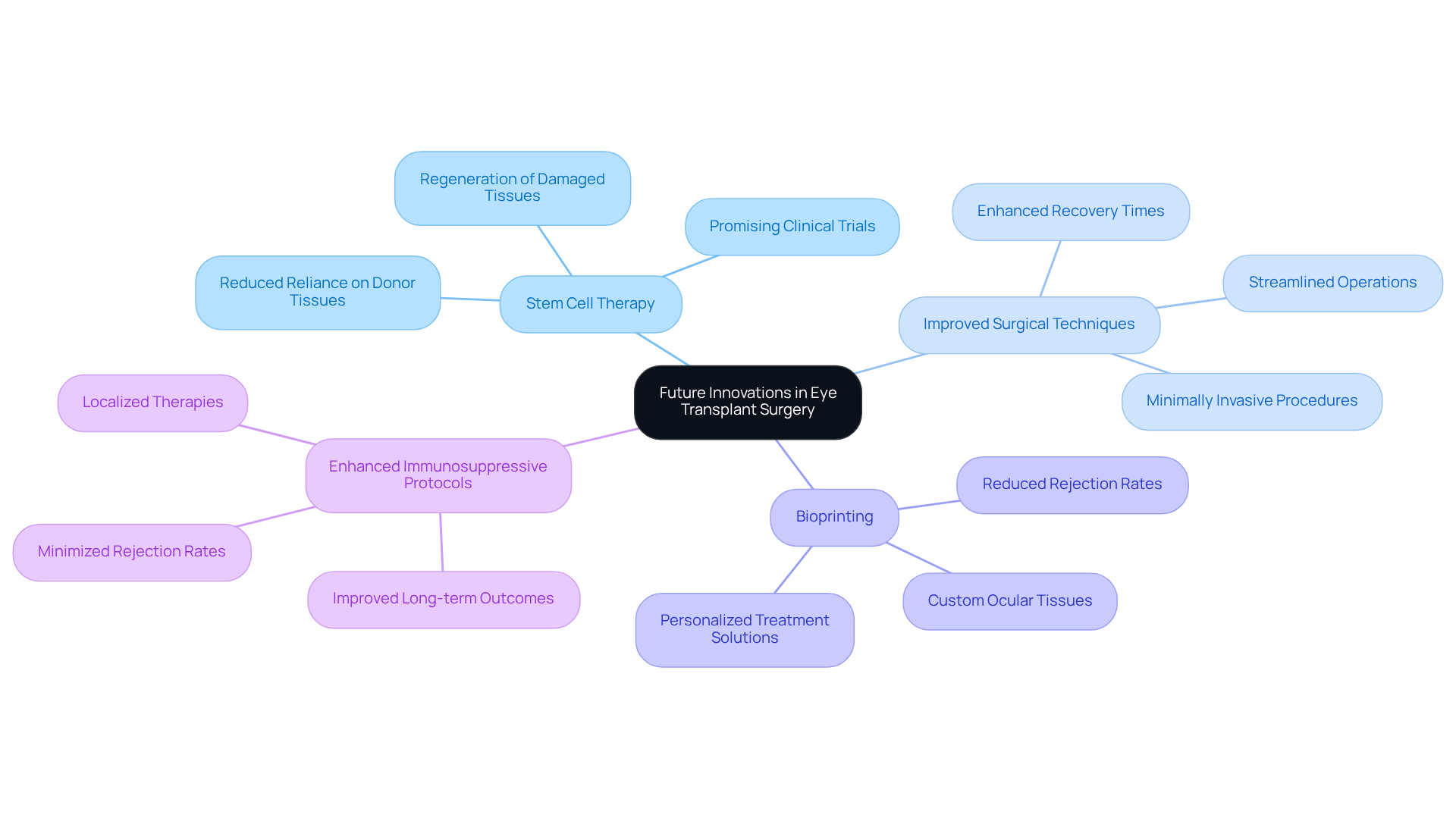
Transformative advancements are on the brink for the future of eye transplant surgery, driven by cutting-edge medical technology and ongoing research. We understand that the journey towards better ocular health can be daunting, but these developments offer hope and reassurance.
-
Stem Cell Therapy: Emerging research highlights the potential of stem cell applications to regenerate damaged eye tissues. This could significantly reduce reliance on donor tissues. Clinical trials have shown promising outcomes, with participants experiencing halted vision loss and some regaining vision after stem cell interventions. This is a beacon of hope for many.
-
Improved Surgical Techniques: Innovations in minimally invasive surgical techniques are set to enhance recovery times and minimize complications associated with eye transplant surgery. These advancements aim to streamline procedures, making them safer and more efficient for individuals. It’s common to feel anxious about surgery, but these improvements can help ease those concerns.
-
Bioprinting: The advent of bioprinting technologies holds the promise of creating custom ocular tissues tailored to individual patient needs. This revolutionary approach could redefine the landscape of eye surgery, offering personalized solutions that enhance compatibility and reduce rejection rates. Imagine a future where your treatment is uniquely designed for you.
-
Enhanced Immunosuppressive Protocols: Ongoing research into more effective immunosuppressive therapies aims to minimize rejection rates and improve long-term outcomes for organ recipients. By refining these protocols, the medical community strives to improve the success rates of eye procedures, ensuring a better quality of life for patients. We are here to help you through this process.
These innovations not only promise to elevate the success rates of eye transplant surgery but also strive to make these vital procedures more accessible to those in need. Ultimately, they aim to transform the future of ocular health, bringing hope and healing to many.
Conclusion
Eye transplant surgery represents a significant advancement in ocular health, offering patients the potential to regain their vision through various procedures, primarily corneal transplants. We understand that the journey to restoring sight can be daunting, and grasping the complexities involved—from pre-operative evaluations to the surgical process and post-operative care—can empower you to make informed decisions about your treatment options. The distinctions between corneal and whole eye transplants highlight the varying levels of complexity and the experimental status of whole eye procedures, underscoring the need for ongoing research and patient education.
Throughout this discussion, we have explored key points such as:
- The importance of donor tissue selection
- The challenges of rejection risks
- The psychological impacts of undergoing such surgeries
The high success rates of corneal transplants, combined with advancements in surgical techniques and innovations like stem cell therapy and bioprinting, paint an optimistic picture for the future of eye transplant surgery. Addressing the limitations and challenges faced in this field is crucial for improving patient outcomes and expanding access to these life-changing procedures.
As the landscape of eye transplant surgery evolves, staying informed about the latest trends and innovations is essential. We understand that you may have concerns about the future, but the pursuit of enhanced surgical methods, improved immunosuppressive therapies, and personalized treatment options aims not only to increase the success rates of these procedures but also to offer hope to those affected by vision loss. Embracing these advancements can pave the way for a future where ocular health is more accessible and effective, ultimately transforming lives and restoring the gift of sight.
Frequently Asked Questions
What is eye transplant surgery?
Eye transplant surgery consists of specialized operations aimed at restoring vision by replacing damaged or diseased eye tissues, particularly through corneal transplants.
What steps are involved in the eye transplant process?
The eye transplant process involves several critical steps: pre-operative evaluation, donor tissue selection, the surgical procedure, and post-operative care.
What happens during the pre-operative evaluation?
During the pre-operative evaluation, a comprehensive examination is conducted to assess your eye health and determine your suitability for transplantation. This helps identify any underlying conditions that may influence the procedure’s success.
Are there any medications I need to stop before the surgery?
Yes, you may need to discontinue specific medications, such as aspirin and ibuprofen, 7 to 10 days prior to the procedure.
How is donor tissue selected for the surgery?
Surgeons carefully select donor tissues that meet stringent compatibility criteria to minimize the risk of rejection and ensure the best possible outcome.
What occurs during the surgical procedure?
The surgical procedure is performed under anesthesia, either general or local. The damaged cornea is meticulously removed and replaced with healthy donor tissue to restore vision.
What post-operative care should I expect after the surgery?
After the procedure, you will receive detailed recovery instructions, including the use of prescribed medications to prevent infection and manage inflammation. A follow-up appointment is necessary the day after the surgery to monitor healing and address any complications.
How common are corneal transplant procedures?
Corneal procedures are the most prevalent form of organ replacement in the U.S., with over 137,000 tissue recoveries recorded in 2023 alone.
How long does it take to recover vision after a corneal transplant?
Many individuals experience notable vision enhancement within weeks, while others may require up to a year for complete recovery.