Posted by: Northwest Eye in General on November 25, 2025
Introduction
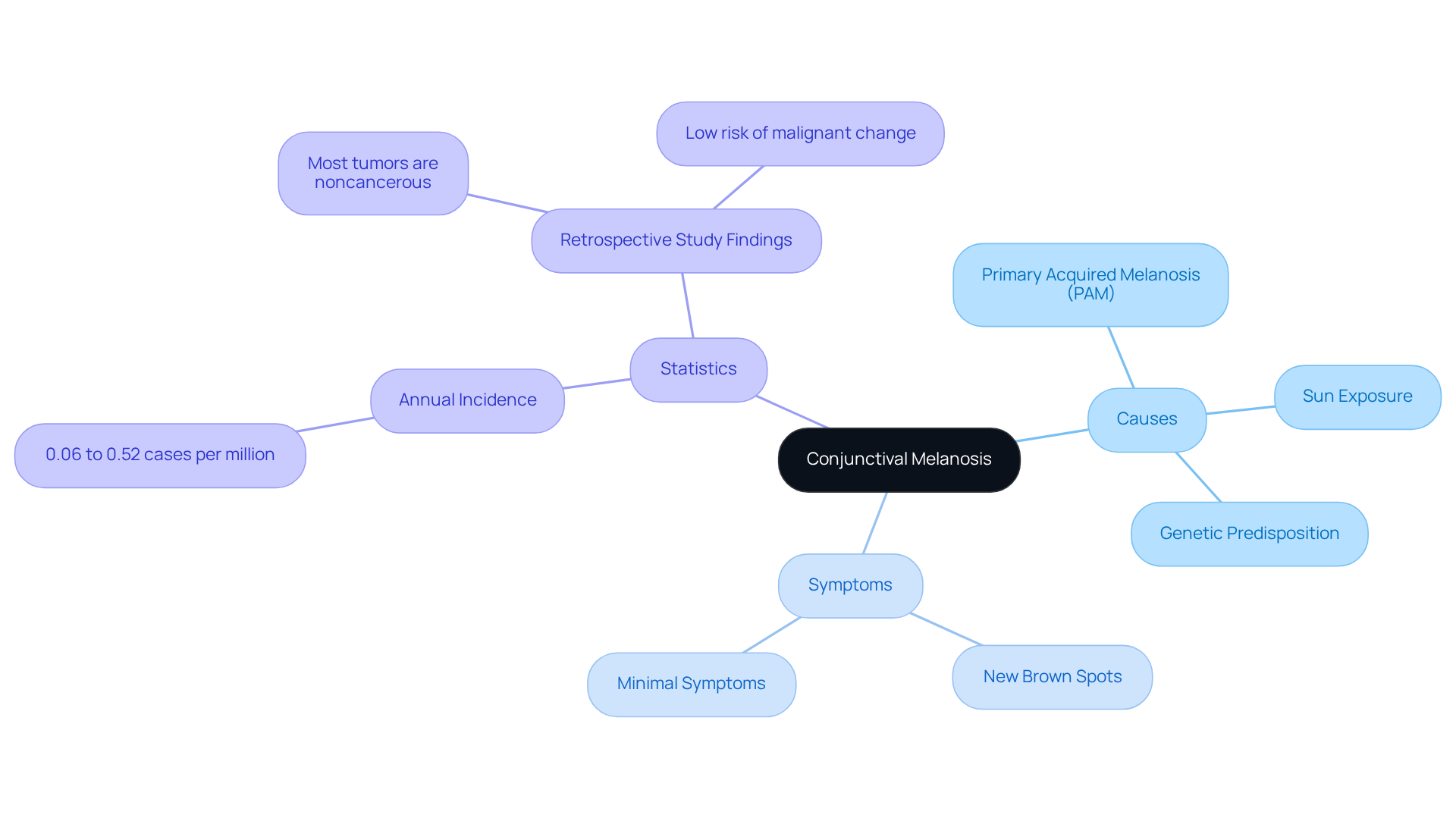
Conjunctival melanosis can be concerning, especially when you notice unsettling brown patches on the surface of your eye. This condition, often referred to as primary acquired melanosis (PAM), is usually benign. However, it does have the potential for malignancy, which is why awareness and early detection are so important.
We understand that it can be overwhelming to navigate the complexities of diagnosis and treatment options. You might be wondering: how can you tell if the pigmentation is harmless or something more serious? Understanding the nuances of conjunctival melanosis is essential for effective management and peace of mind.
It’s common to feel anxious about these changes, but remember, you’re not alone in this journey. Many individuals have faced similar concerns and found reassurance through understanding their condition better. We are here to help you through this process.
Define Conjunctival Melanosis: Causes and Symptoms
Conjunctival melanosis can be concerning, as it often appears as flat, brown patches on the conjunctiva. We understand that noticing these changes can be unsettling. The primary cause is usually conjunctival melanosis, also known as primary acquired melanosis (PAM), a non-cancerous condition that can sometimes progress to malignancy, typically affecting one eye. Other factors, such as sun exposure and genetic predisposition, can also play a role.
While symptoms may be minimal, many patients notice new brown spots or patches on their conjunctiva. It’s important to differentiate between harmless conjunctival melanosis and potentially harmful growths. Early identification can significantly impact treatment outcomes, and we want to reassure you that monitoring these changes is crucial.
Recent studies, particularly those from Scandinavia, reveal that the annual incidence of eye melanoma is quite rare, ranging from 0.06 to 0.52 cases per million. This highlights the importance of keeping an eye on any changes. For instance, a retrospective study involving over 3,300 patients with eye surface abnormalities found that most tumors are noncancerous, with a low risk of malignant change.
Ophthalmologists, including experts like Lauren A. Dalvin, M.D., stress the importance of vigilance in monitoring any pigmentation changes. Remember, timely intervention can lead to better management of your condition. We are here to help you through this process and ensure you receive the care you need.
Diagnose Conjunctival Melanosis: Key Techniques and Considerations
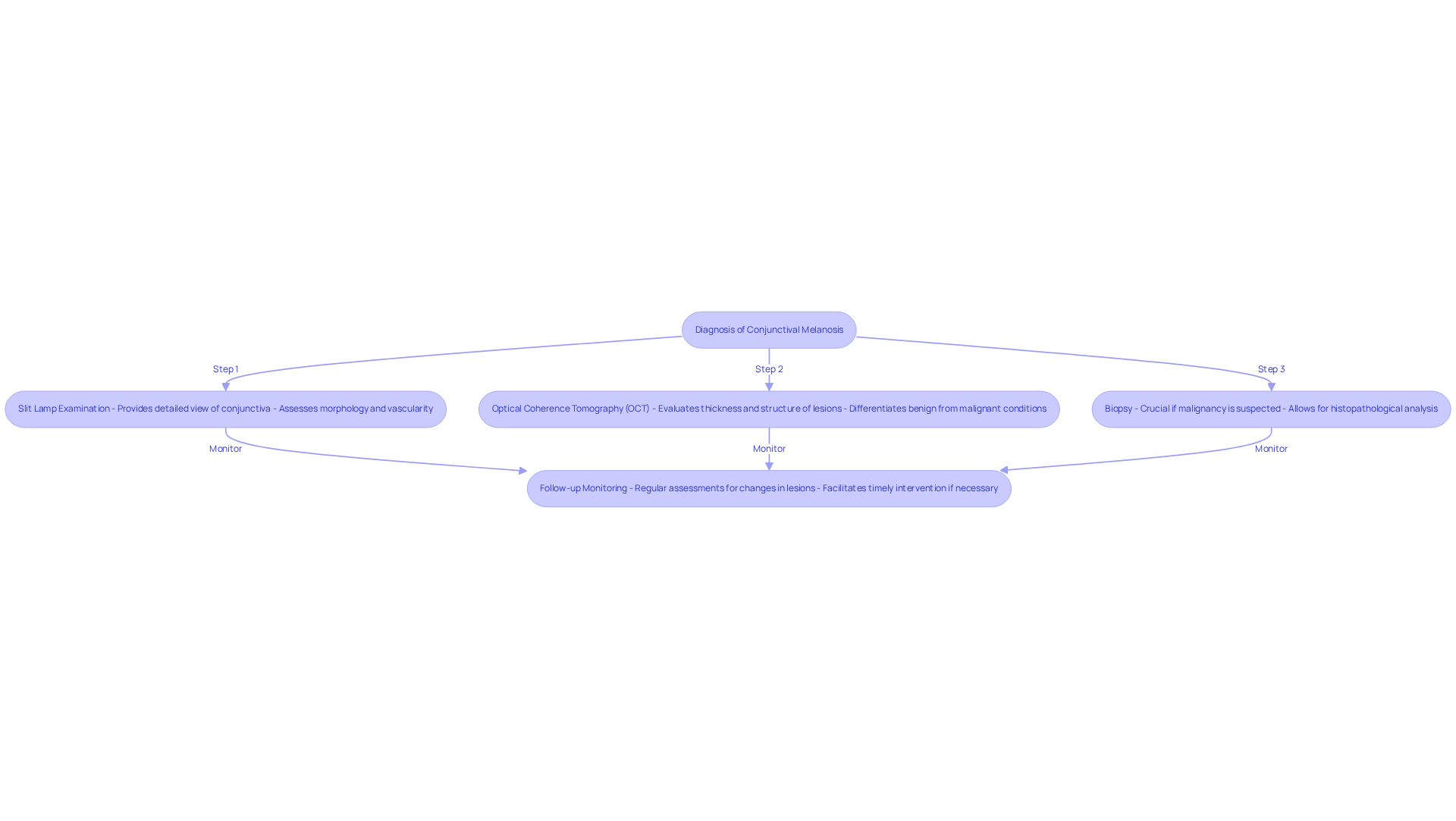
Identifying conjunctival melanosis in the eye can feel overwhelming, but we’re here to guide you through the process. A comprehensive examination is essential, and a slit lamp is often used to carefully assess the features of the spots. Here are some key diagnostic techniques that can help:
- Slit Lamp Examination: This method provides a detailed view of the conjunctiva and any pigmented lesions. It allows for a thorough assessment of their morphology and vascularity, giving you and your doctor valuable insights.
- Optical Coherence Tomography (OCT): This advanced imaging technique evaluates the thickness and structural integrity of eye lesions. It offers high-resolution images that can help differentiate between non-cancerous and malignant conditions. Experts note that ‘AS-OCT has shown great promise in the diagnosis and treatment of benign and malignant eye surface pathologies.’
- Biopsy: If there’s a suspicion of malignancy, a biopsy becomes crucial. This procedure allows for tissue samples to be obtained for histopathological analysis, which is vital for distinguishing between primary acquired pigmentation (PAM) and conjunctival melanosis or melanoma of the eye. This ensures that the right management strategies are applied.
We understand that regular follow-ups can feel daunting, but they are crucial for monitoring any changes in the lesions over time. This proactive approach facilitates timely intervention if necessary. By incorporating these diagnostic methods, we can enhance the precision of eye tissue assessments, ultimately improving patient outcomes. Furthermore, studies suggest that the average rate of lymph node metastasis in ocular malignant melanoma (CMM) is around 19%. This highlights the importance of early detection and ongoing monitoring. Remember, we are here to help you through this process.
Treat Conjunctival Melanosis: Options and Best Practices
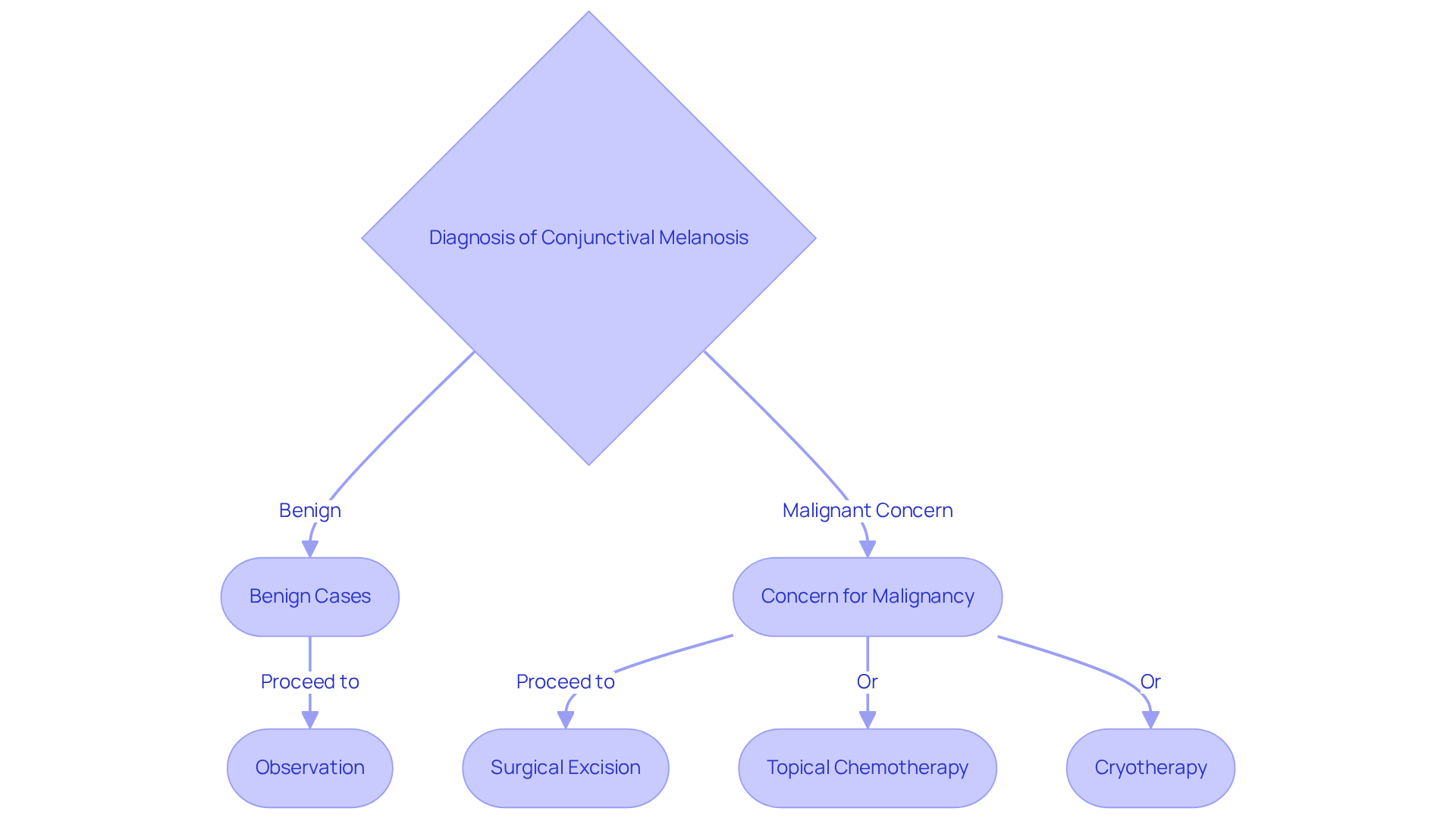
We understand that you may have concerns about the potential risks and the best treatment options when it comes to managing conjunctival melanosis. Treatment is guided by the diagnosis and the risk of progression to malignancy, and we want to ensure you feel informed and supported throughout this process. Here are some common options to consider:
- Observation: For benign cases, regular monitoring is often sufficient, especially if the lesions remain stable. This approach allows for timely intervention if any changes occur, giving you peace of mind.
- Surgical Excision: If there’s concern for malignancy or if the growths are causing symptoms, surgical removal is typically recommended. This procedure involves excising the lesion with clear margins to ensure complete removal, which is crucial for preventing recurrence. Studies indicate that surgical excision can achieve success rates of up to 80% in managing conjunctival melanoma, underscoring its effectiveness in eliminating malignant cells. Additionally, the success rate of strontium-90 as adjuvant therapy ranges from 43% to 90%, providing context for the effectiveness of surgical excision compared to other treatments.
- Topical Chemotherapy: In cases of primary acquired melanosis (PAM) with atypia, topical agents like mitomycin C may be utilized to reduce the risk of progression to melanoma. This treatment has shown a high success rate of 86.4% in decreasing unusual growths, which can be reassuring.
- Cryotherapy: This method is used for larger abnormalities that cannot be entirely removed. It involves freezing the affected area to destroy abnormal cells, offering an alternative for patients who may not be candidates for surgery.
Each treatment plan should be customized, taking into account factors such as the characteristics of the lesions, your age, and overall health. We encourage regular follow-ups and thorough examinations to monitor conjunctival melanosis, ensuring prompt action if malignancy is suspected. Remember, we are here to help you through this process.
Conclusion
Conjunctival melanosis, especially primary acquired melanosis (PAM), can be concerning. These flat brown patches on the conjunctiva require careful monitoring because they have the potential to progress to malignancy. We understand that this can be alarming, but recognizing the nature of these lesions is crucial. Early detection and intervention can significantly influence treatment outcomes, and being vigilant about any changes can empower you to manage your eye health effectively.
In this article, we outline essential diagnostic techniques that can help ease your worries.
- Slit lamp examinations
- Optical coherence tomography (OCT)
- Biopsies
These are vital for distinguishing between benign and malignant conditions. Regular follow-ups and comprehensive assessments are emphasized to ensure timely intervention if any changes occur. Treatment options, such as observation, surgical excision, topical chemotherapy, and cryotherapy, offer tailored approaches based on your individual circumstances and the characteristics of the lesions.
Ultimately, awareness and education about conjunctival melanosis are paramount for effective management. We encourage you to remain vigilant about any changes in your eye health and to consult with healthcare professionals for personalized care. By prioritizing regular eye examinations and staying informed about the latest advancements in treatment options, you can navigate the complexities of conjunctival melanosis with confidence. Remember, we are here to help you through this process, ensuring optimal outcomes for your eye health.
Frequently Asked Questions
What is conjunctival melanosis?
Conjunctival melanosis, also known as primary acquired melanosis (PAM), is a non-cancerous condition characterized by flat, brown patches on the conjunctiva, which can sometimes progress to malignancy.
What causes conjunctival melanosis?
The primary cause is usually conjunctival melanosis itself, but factors such as sun exposure and genetic predisposition can also contribute to its development.
What are the symptoms of conjunctival melanosis?
Symptoms may be minimal, but many patients notice new brown spots or patches on their conjunctiva.
Why is it important to monitor changes in conjunctival melanosis?
Early identification of changes can significantly impact treatment outcomes, as it is crucial to differentiate between harmless conjunctival melanosis and potentially harmful growths.
How common is eye melanoma?
Recent studies indicate that the annual incidence of eye melanoma is quite rare, ranging from 0.06 to 0.52 cases per million.
What do studies suggest about the risk of malignant change in conjunctival melanosis?
A retrospective study involving over 3,300 patients with eye surface abnormalities found that most tumors are noncancerous, with a low risk of malignant change.
What do ophthalmologists recommend regarding pigmentation changes?
Ophthalmologists stress the importance of vigilance in monitoring any pigmentation changes, as timely intervention can lead to better management of the condition.