Posted by: Northwest Eye in General on November 21, 2025
Introduction
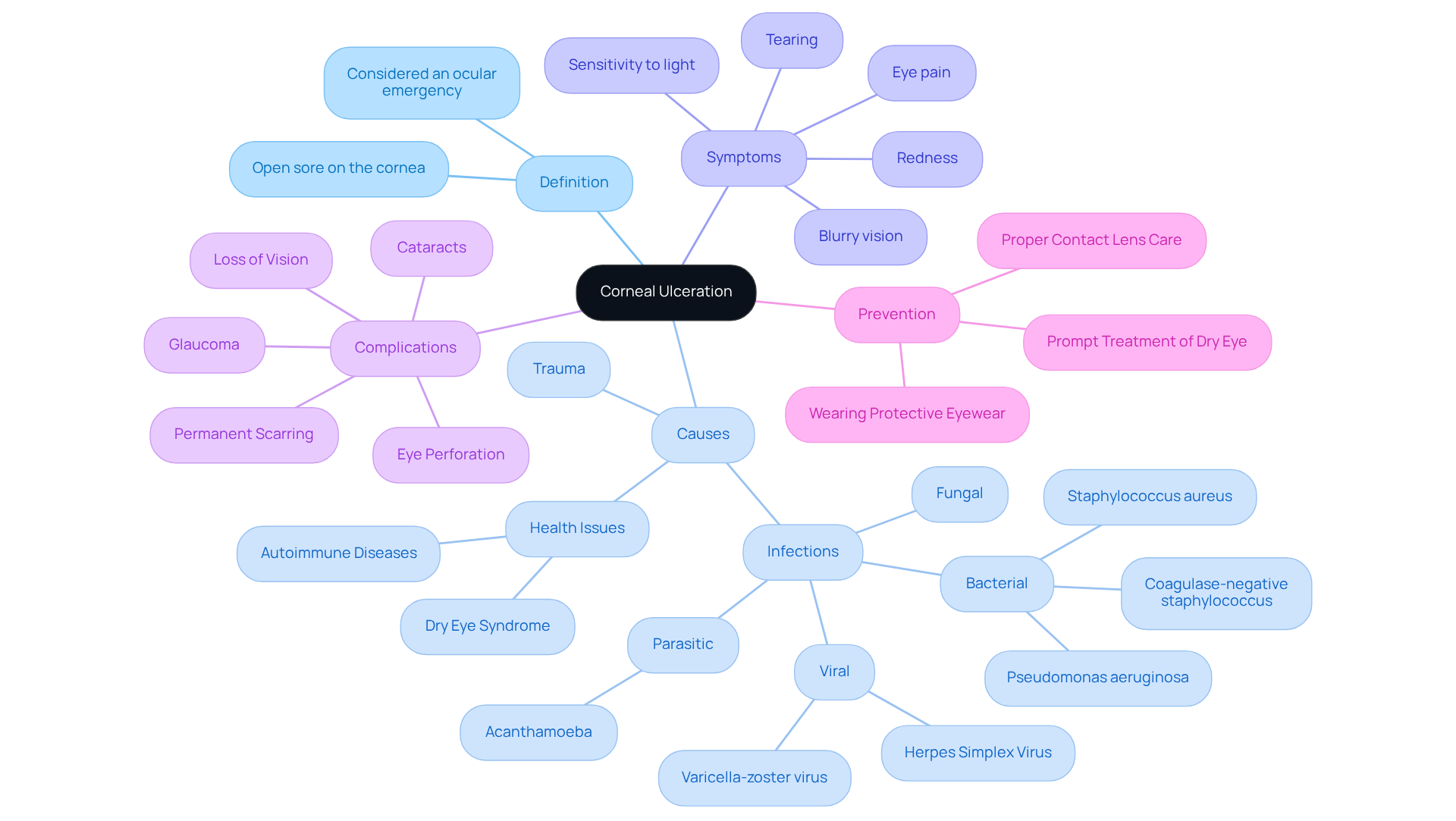
Understanding the complexities of corneal ulceration is crucial for anyone who cares about their eye health. This condition, marked by painful open sores on the cornea, can stem from various causes like infections, trauma, or underlying health issues. If not addressed promptly, it poses a significant threat to vision.
As we see more cases of corneal ulcers, recognizing the symptoms and knowing the treatment options can empower you to seek timely medical help. We understand that it can be overwhelming to navigate this situation. So, what are the key signs to look out for? And how can you effectively manage the complexities of diagnosis and treatment?
It’s common to feel anxious about your eye health, but remember, you are not alone in this journey. We are here to help you through this process.
Define Corneal Ulceration: An Overview of the Condition
A corneal abrasion, often called keratitis, is an open sore on the cornea, the clear, protective outer layer of your eye. We understand that discovering you have this condition can be concerning. Corneal abrasions can happen for various reasons, including infections, trauma, or underlying health issues. It’s important to know that these lesions are considered ocular emergencies because they can threaten your vision if not treated promptly.
These abrasions can manifest as either superficial corneal ulceration or deep corneal ulceration. Deep ulcers pose a greater risk of complications, such as eye perforation or scarring. In fact, statistics reveal that keratitis, which can lead to corneal ulceration, accounts for about one million visits to clinics and emergency departments each year in the United States. This highlights the broader impact of related conditions and the importance of understanding corneal ulceration.
Recognizing the symptoms of corneal ulceration is crucial for seeking timely medical help. Eye specialists emphasize that corneal ulceration on the eye’s surface indicates a serious visual emergency that could lead to vision-threatening complications. Common bacterial pathogens linked to eye infections include:
- Staphylococcus aureus
- Coagulase-negative staphylococcus
- Pseudomonas aeruginosa
To lower the risk of developing eye sores, preventive actions are essential. Proper contact lens care, wearing protective eyewear, and addressing dry eye and eyelid conditions promptly can make a significant difference. Remember, untreated eye lesions can lead to:
- Permanent scarring of the cornea
- Eye perforation
- Loss of vision or blindness
- Glaucoma
- Cataracts
- Irregular astigmatism
- Severe inflammation of the eye
We are here to help you through this process. If you have any concerns or questions, don’t hesitate to reach out for support.
Identify Causes: Understanding the Triggers of Corneal Ulcers
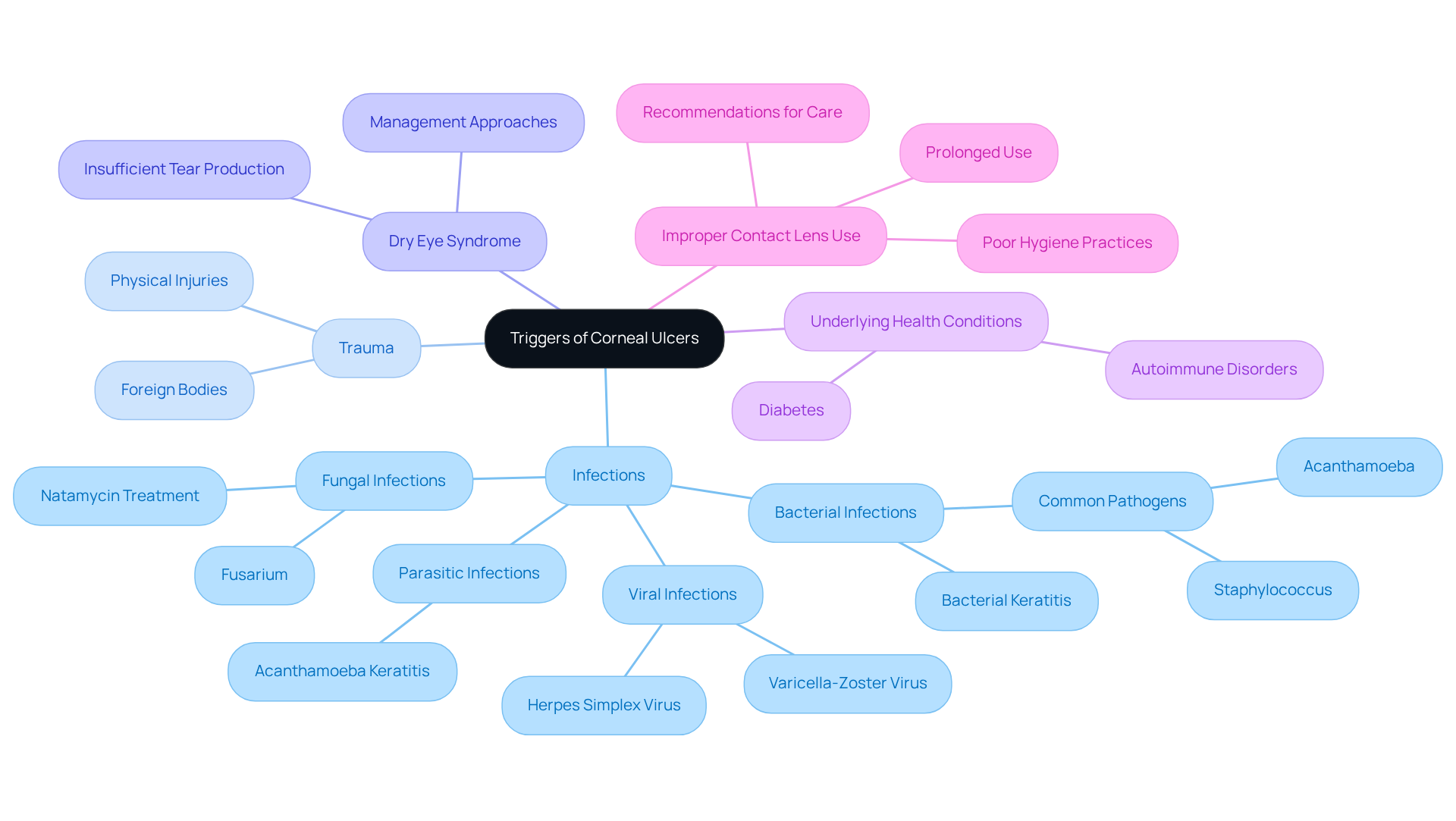
Corneal ulceration can arise from various factors, each contributing to the risk of developing ulcers. We understand that this can be concerning, so let’s explore these factors together:
-
Infections: Bacterial, viral (notably herpes simplex), fungal, and parasitic infections play a significant role in corneal ulcers. For instance, bacterial keratitis is especially common among contact lens wearers, where improper hygiene practices can heighten this risk. Research indicates that microbial keratitis leads to about 930,000 outpatient visits each year, highlighting the strain on healthcare linked to these conditions.
-
Trauma: Physical injuries to the eye, such as scratches or foreign bodies, can disrupt the surface of the eye and lead to ulceration. It’s common to feel anxious about such injuries, but understanding them can help.
Dry Eye Syndrome occurs when insufficient tear production compromises the cornea’s protective barrier, making it more vulnerable to infections and resulting in corneal ulceration. Many individuals with eye lesions experience dry eye syndrome, emphasizing the need for effective management approaches to reduce this risk.
-
Underlying Health Conditions: Chronic ailments like diabetes and autoimmune disorders can hinder healing processes, increasing the chance of developing eye sores. We recognize that managing these conditions can be challenging.
-
Improper Contact Lens Use: Prolonged use of contact lenses, especially without adequate hygiene, greatly increases the risk of eye infections. Health organizations recommend adhering to proper lens care practices to prevent infections, and we are here to support you in this.
Understanding these triggers is essential for effective prevention and management of corneal ulceration, especially for those at increased risk, such as contact lens wearers. Additionally, recognizing that the cornea is a transparent dome-shaped layer covering the pupil and iris, and understanding the balance of fluid movement in the cornea, underscores its importance in overall eye health. We are here to help you through this process.
Recognize Symptoms: Key Indicators of Corneal Ulceration
The severity of symptoms related to corneal ulceration can vary, and we understand how concerning they can be. Here are some common signs to watch for:
- Severe Eye Pain: This is often described as a sharp or throbbing sensation. Severe eye pain is a hallmark symptom of corneal ulceration, and it can be debilitating. If you’re experiencing this, it’s important to seek medical attention promptly.
- Redness and Inflammation: You might notice that the affected eye appears red and swollen, indicating inflammation. This is your body’s way of reacting to illness or injury, and ongoing redness should not be ignored.
- Discharge: If you see pus or watery discharge, it could signal an underlying infection. This symptom is particularly concerning and warrants immediate evaluation by an eye care professional.
- Blurred or Hazy Vision: Damage to the eye’s surface can lead to blurred or hazy sight, significantly interfering with daily activities. If your vision is unclear, it’s essential to seek immediate medical care.
- Sensitivity to Light: Heightened sensitivity to bright lights, known as photophobia, is common in cases of eye lesions. You may find yourself squinting or avoiding bright environments due to discomfort.
- Foreign Body Sensation: Many people describe a feeling as if something is stuck in their eye. This can be troubling and may suggest irritation or injury.
- Chronic Itching and Watery Eyes: These symptoms can also occur and should be monitored closely.
Recognizing these symptoms early is crucial. Timely intervention can prevent complications, such as permanent vision loss, which occurs in about 20% of untreated cases. We understand that any signs of severe eye pain or changes in vision can be alarming. It’s important to seek immediate medical evaluation to ensure the best possible outcomes. If you’re experiencing any of these symptoms, please schedule an appointment with a Northwest Eye doctor for a thorough examination. We are here to help you through this process.

Diagnose Corneal Ulcers: Methods and Importance of Accurate Assessment
Diagnosing corneal ulceration can feel overwhelming, but understanding the process can help ease your concerns. Here’s what to expect:
- Patient History: We start by gathering detailed information about your symptoms, contact lens usage, and any recent eye injuries. This context is essential for an accurate diagnosis.
- Slit-Lamp Examination: Using a specialized microscope called a slit lamp, your ophthalmologist will closely examine your cornea. This examination is crucial, as research shows it achieves accuracy rates over 90% in diagnosing eye lesions. For instance, a recent study highlighted that a CNN model reached accuracy rates of 95.77%, 96.43%, and 97.27% in classifying corneal conditions. This underscores the effectiveness of advanced diagnostic tools alongside traditional methods.
- Fluorescein Staining: This technique involves applying a fluorescent dye to your eye, which highlights any damaged areas on the cornea. This makes corneal ulceration more visible, which aids in accurate diagnosis.
- Microbial Cultures: If an infection is suspected, cultures may be taken from any eye discharge to identify the causative organism. This ensures you receive the appropriate treatment.
Accurate diagnosis through these methods is vital. It informs your treatment plan and helps prevent serious complications, including vision loss. The slit-lamp examination, in particular, is essential for evaluating the health of your eye’s surface and plays a vital role in comprehensive eye care. As experts in the field emphasize, “Timely diagnosis and prompt referral to subspecialty care is crucial to optimize clinical outcomes, particularly in underserved communities where emergency department utilization is high.”
We understand that facing these procedures can be daunting, but remember, we are here to help you through this process. Your health and comfort are our top priorities.
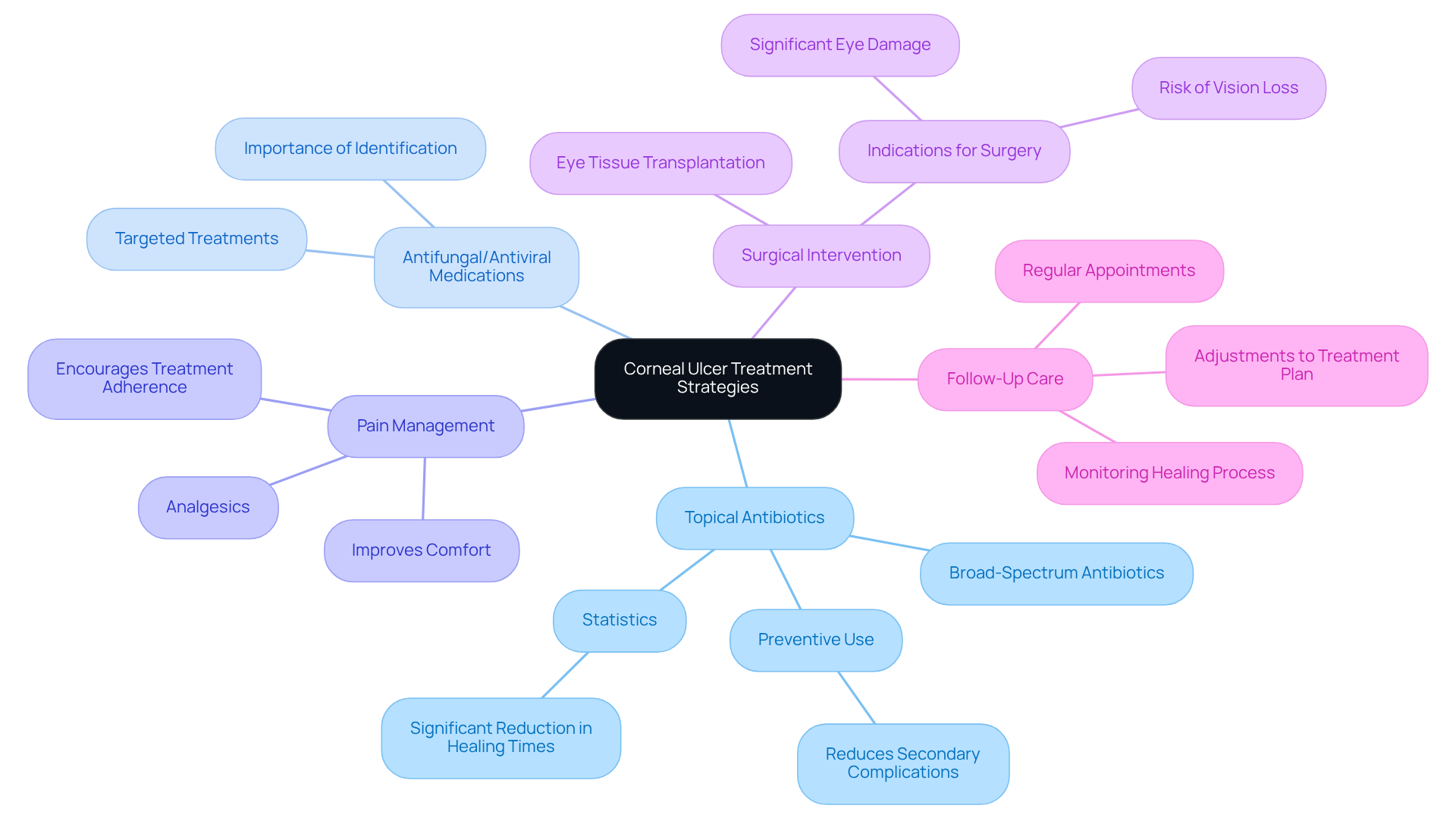
Treat Corneal Ulcers: Comprehensive Management Strategies
Efficient handling of eye tissue lesions is essential, and we understand that this can be a concerning experience for you. The approach to treatment varies based on the root cause, and we’re here to guide you through it. Here are the primary treatment strategies:
-
Topical Antibiotics: Broad-spectrum antibiotics are often prescribed to tackle bacterial infections linked to corneal ulcers. These medications are typically administered multiple times daily to ensure adequate coverage and promote healing. Research shows that the preventive use of topical antibiotics can significantly lower the likelihood of secondary complications, which are common in cases of corneal ulceration.
-
Antifungal or Antiviral Medications: If fungal or viral ailments are identified as the cause, specific antifungal or antiviral treatments are utilized. This targeted approach is crucial for effectively managing the infection and facilitating your recovery.
-
Pain Management: We know that discomfort can be distressing, so analgesics are often recommended to alleviate pain associated with corneal ulceration. Effective pain management not only improves your comfort but also encourages adherence to treatment protocols.
-
Surgical Intervention: In critical situations where conservative therapies aren’t effective, surgical options like eye tissue transplantation may be necessary. Surgical intervention is usually considered when there is significant eye damage or a risk of vision loss.
-
Follow-Up Care: Regular follow-up appointments are vital for monitoring your healing process and making necessary adjustments to your treatment plan. These evaluations help ensure that any complications are promptly addressed, preserving your vision.
Real-world examples highlight the importance of these strategies. For instance, a study involving 40 patients demonstrated that those receiving comprehensive management, including topical antibiotics, experienced a significant reduction in healing times and improved visual acuity. Furthermore, 93.3% of patients treated with amniotic membrane transplantation (AMT) achieved healing compared to 76.7% in control groups, underscoring the effectiveness of advanced treatment options.
Expert opinions reinforce the significance of timely intervention. Ophthalmologists emphasize that early diagnosis and appropriate antibiotic treatment are critical in preventing complications and ensuring successful outcomes. Statistics indicate that visual sharpness enhanced in 47% of instances treated with AMT, versus 33% in those undergoing standard care, emphasizing the possible advantages of innovative therapies in managing eye conditions.
In summary, a multifaceted approach that includes topical antibiotics, pain management, and regular follow-up is essential for effectively treating corneal ulceration and preserving your vision. We are here to help you through this process.
Conclusion
Understanding corneal ulceration is crucial for maintaining your eye health and preventing potential complications. This condition, which presents as an open sore on the cornea, can arise from various causes, including infections, trauma, and underlying health issues. We understand that recognizing the urgency of corneal ulceration as an ocular emergency is vital, and it underscores the need for awareness and prompt action.
Throughout this article, we’ve explored the various aspects of corneal ulceration, from its causes and symptoms to diagnosis and treatment strategies. It’s important to identify symptoms like severe eye pain, redness, and discharge. Proper contact lens care and managing underlying health conditions play a significant role in prevention. Additionally, accurate diagnosis through methods such as slit-lamp examination and fluorescein staining is essential for effective treatment, which may involve antibiotics, antifungal medications, and even surgical interventions when necessary.
The significance of understanding corneal ulceration cannot be overstated. By being informed about the causes, symptoms, and treatment options, you can take proactive steps to protect your vision. Early intervention and adherence to recommended care practices are essential in preventing severe complications, including vision loss. It’s common to feel anxious at the first sign of symptoms, but seeking medical attention promptly can make a significant difference in outcomes.
We are here to help you through this process. By taking the time to understand corneal ulceration, you empower yourself to act decisively. Remember, early action is key to preserving your vision and ensuring your eye health.
Frequently Asked Questions
What is a corneal ulceration?
A corneal ulceration, also known as keratitis, is an open sore on the cornea, the clear outer layer of the eye. It can occur due to infections, trauma, or underlying health issues and is considered an ocular emergency that can threaten vision if not treated promptly.
What are the types of corneal ulceration?
Corneal ulceration can manifest as either superficial or deep. Deep corneal ulcers pose a greater risk of complications, such as eye perforation or scarring.
What are the common causes of corneal ulceration?
Common causes include infections (bacterial, viral, fungal, and parasitic), trauma to the eye, dry eye syndrome, underlying health conditions (like diabetes and autoimmune disorders), and improper contact lens use.
What are the symptoms of corneal ulceration?
Symptoms of corneal ulceration can include pain, redness, blurred vision, tearing, and sensitivity to light. Timely medical help is crucial if these symptoms are present.
What are the risks of untreated corneal ulceration?
Untreated corneal ulceration can lead to permanent scarring of the cornea, eye perforation, loss of vision or blindness, glaucoma, cataracts, irregular astigmatism, and severe inflammation of the eye.
How can corneal ulceration be prevented?
Preventive measures include proper contact lens care, wearing protective eyewear, and addressing dry eye and eyelid conditions promptly. Maintaining good hygiene practices is essential, especially for contact lens wearers.
How prevalent is keratitis and corneal ulceration?
Keratitis, which can lead to corneal ulceration, accounts for about one million visits to clinics and emergency departments each year in the United States, highlighting its significant impact on public health.