Posted by: Northwest Eye in General on September 28, 2025
Overview
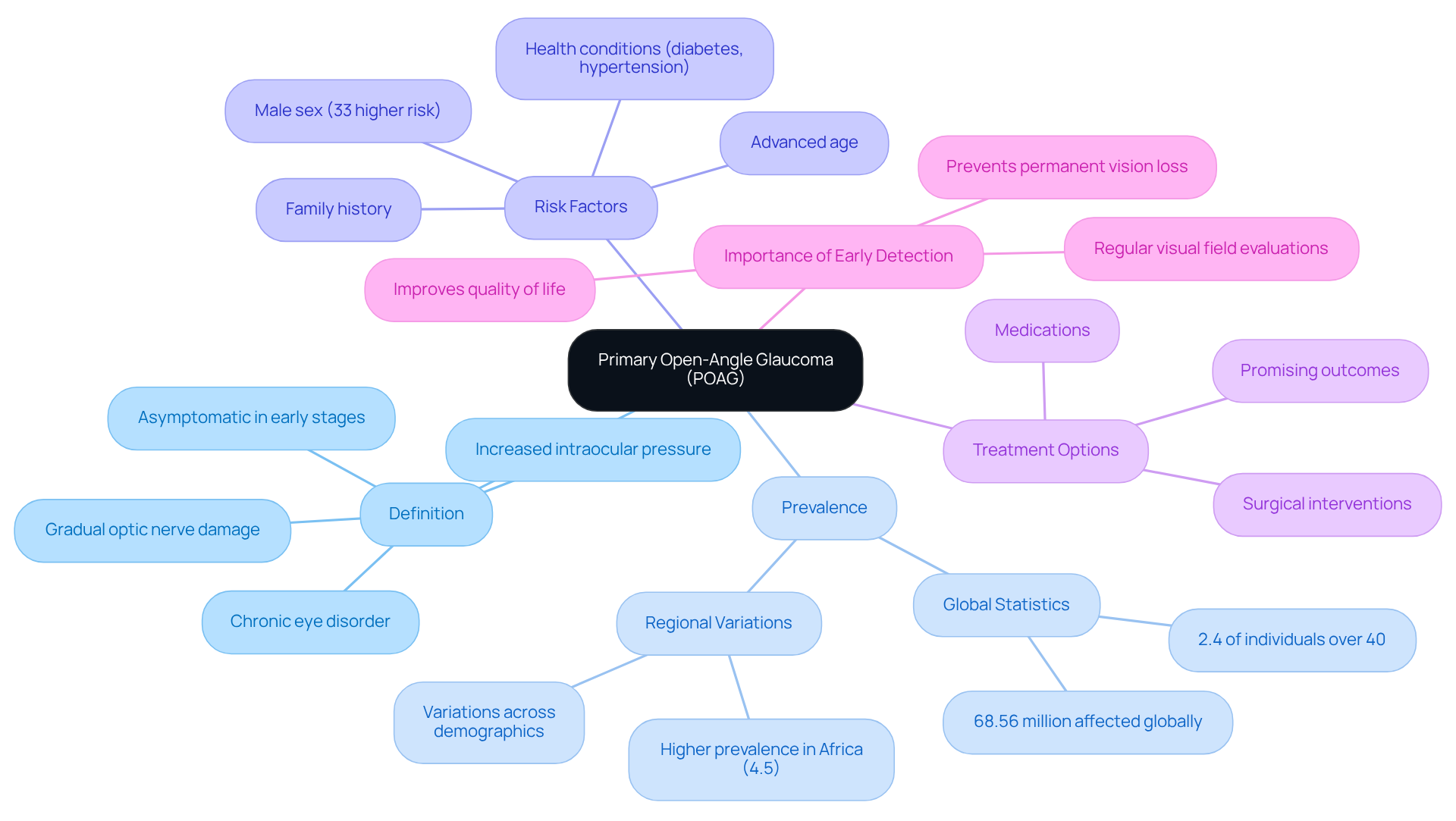
Primary Open-Angle Glaucoma (POAG) is a chronic eye condition that can feel overwhelming, as it is characterized by gradual optic nerve damage, often due to elevated intraocular pressure. It’s often referred to as a “sneak thief of sight” because it typically presents without symptoms in its early stages, leaving many unaware of its presence.
We understand that learning about POAG can be concerning. Key symptoms to look out for include:
- Peripheral vision loss
- Halos around lights
Additionally, factors such as age and family history can increase your risk. Knowing this can help you feel more informed and empowered about your eye health.
It’s important to know that there are various treatment options available, including medications and laser therapy. Early detection is crucial, and we encourage you to prioritize regular eye exams. Taking these steps can significantly help in preventing severe vision loss. Remember, we are here to help you through this process and support you every step of the way.
Introduction
Primary Open-Angle Glaucoma (POAG) is often referred to as the “sneak thief of sight,” quietly threatening your vision without noticeable symptoms in its early stages. We understand that this can be concerning. With approximately 2.4% of individuals over 40 affected globally, being aware of its symptoms and risk factors is critical for early detection and intervention.
How can you navigate the complexities of POAG treatment while understanding how this condition impacts your daily life?
This article delves into the essentials of POAG, from its symptoms and treatment options to the key risk factors that deserve your attention, empowering you to take proactive steps toward preserving your vision.
Define Primary Open-Angle Glaucoma (POAG)
POAG, or Primary Open-Angle Glaucoma, is a long-lasting eye disorder that can be concerning, as it involves gradual harm to the optic nerve, often linked to increased intraocular pressure. We understand that learning about this condition can be overwhelming, especially since the anterior chamber angle remains open, indicating that the drainage canals are not physically blocked. This is the most common type of glaucoma, often referred to as the ‘sneak thief of sight’ due to its asymptomatic nature in the early stages.
Research shows that approximately 2.4% of individuals over 40 years old globally are affected by primary open-angle glaucoma, with notable variations across different regions and demographics. For instance, the prevalence is higher in Africa, reaching up to 4.5%. If left untreated, this condition can lead to permanent vision loss and blindness, which underscores the importance of early detection and management.
It’s common to feel anxious about the risk factors associated with POAG. These include:
- Advanced age
- Male sex—where men have a 33% higher risk compared to women
- Family history
- Health conditions such as diabetes and hypertension
All of which are risk factors for POAG. We want to reassure you that are available. Medications and surgical interventions have shown promising outcomes in managing the disease and preserving vision.
Patients who receive timely treatment often report improved visual function and a better quality of life. This highlights the critical role of proactive eye care in combating this silent threat to sight. Furthermore, regular visual field evaluations are essential for accurately diagnosing POAG, which stands for primary open-angle glaucoma. We are here to help you through this process, emphasizing the necessity for thorough eye examinations to ensure your well-being.
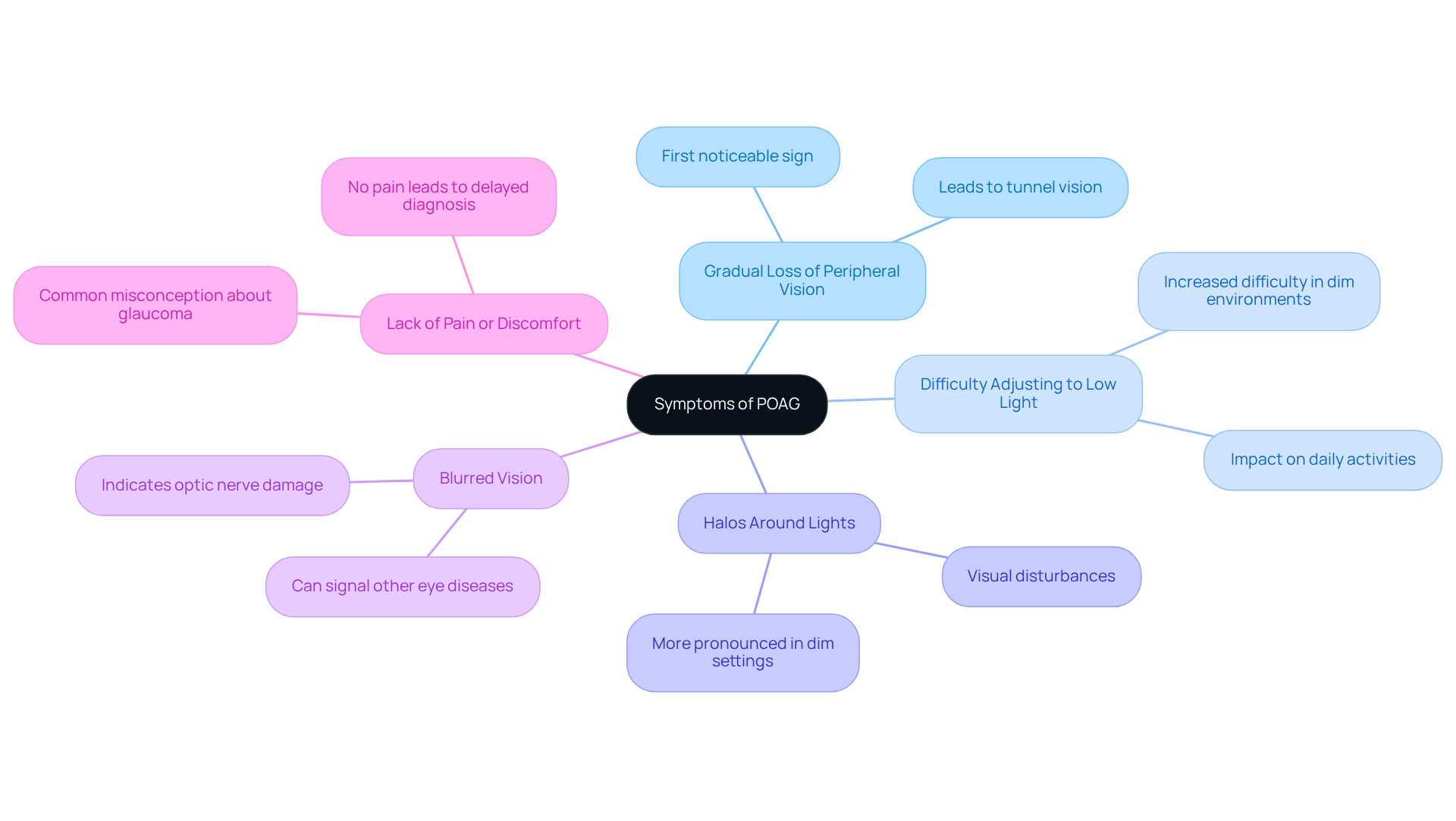
Identify Symptoms of POAG
Primary open-angle glaucoma, or poag, often progresses quietly in its initial phases, making it challenging for individuals to recognize its presence. As the condition advances, you may begin to notice several important symptoms:
- Gradual loss of peripheral vision: This is typically the first noticeable sign, leading to a constricted field of vision often described as tunnel vision.
- Difficulty adjusting to low light: Many individuals report increased difficulty seeing in dimly lit environments, which can significantly impact daily activities.
- Halos around lights: Some people experience visual disturbances, such as halos or rainbow-colored circles surrounding bright lights, which can be disorienting. Halos are often more pronounced in dim or dark settings and can indicate deeper issues, making it essential to consult a professional.
- Blurred vision: As optic nerve damage progresses, blurred vision may occur, further complicating visual clarity. This lack of sharpness can stem from various abnormalities, including uncorrected refractive errors, cataracts, and diabetic retinopathy. It may also signal the presence of other eye diseases. Symptoms left untreated can lead to serious health complications, underscoring the need for timely medical intervention.
- Lack of pain or discomfort: Unlike other eye issues, primary open-angle glaucoma typically does not manifest with pain, which can lead to delays in diagnosis and treatment.
Recognizing these symptoms is crucial for timely intervention, as early detection of poag can significantly improve management outcomes. We understand that it can be concerning to think about these signs, especially for those over 60 or with a . In fact, the prevalence of POAG is reported to be 1.86% in individuals older than 40 years. Many patients have shared their experiences, highlighting the importance of regular eye exams, as they were often unaware of their condition until significant vision loss had occurred. Understanding how peripheral vision loss manifests in POAG can empower you to seek assistance earlier, ultimately preserving your quality of life. Furthermore, the intraocular pressure (IOP) threshold for glaucoma diagnosis is above 22 mmHg, which is essential for understanding the clinical features of primary open-angle glaucoma.
The economic impact of glaucoma is significant, with an estimated annual burden of $2.86 billion in the U.S. This underscores the broader implications of the disease and the importance of awareness and early intervention. Moreover, untreated primary open-angle glaucoma (poag) can lead to permanent vision impairment, making it crucial for you to identify these signs and pursue prompt medical consultation. We are here to help you through this process.
Explore Treatment Options for POAG
Managing POAG is a journey that focuses on reducing intraocular pressure and protecting your optic nerve. We understand that navigating treatment options can feel overwhelming, so let’s explore what’s available together.
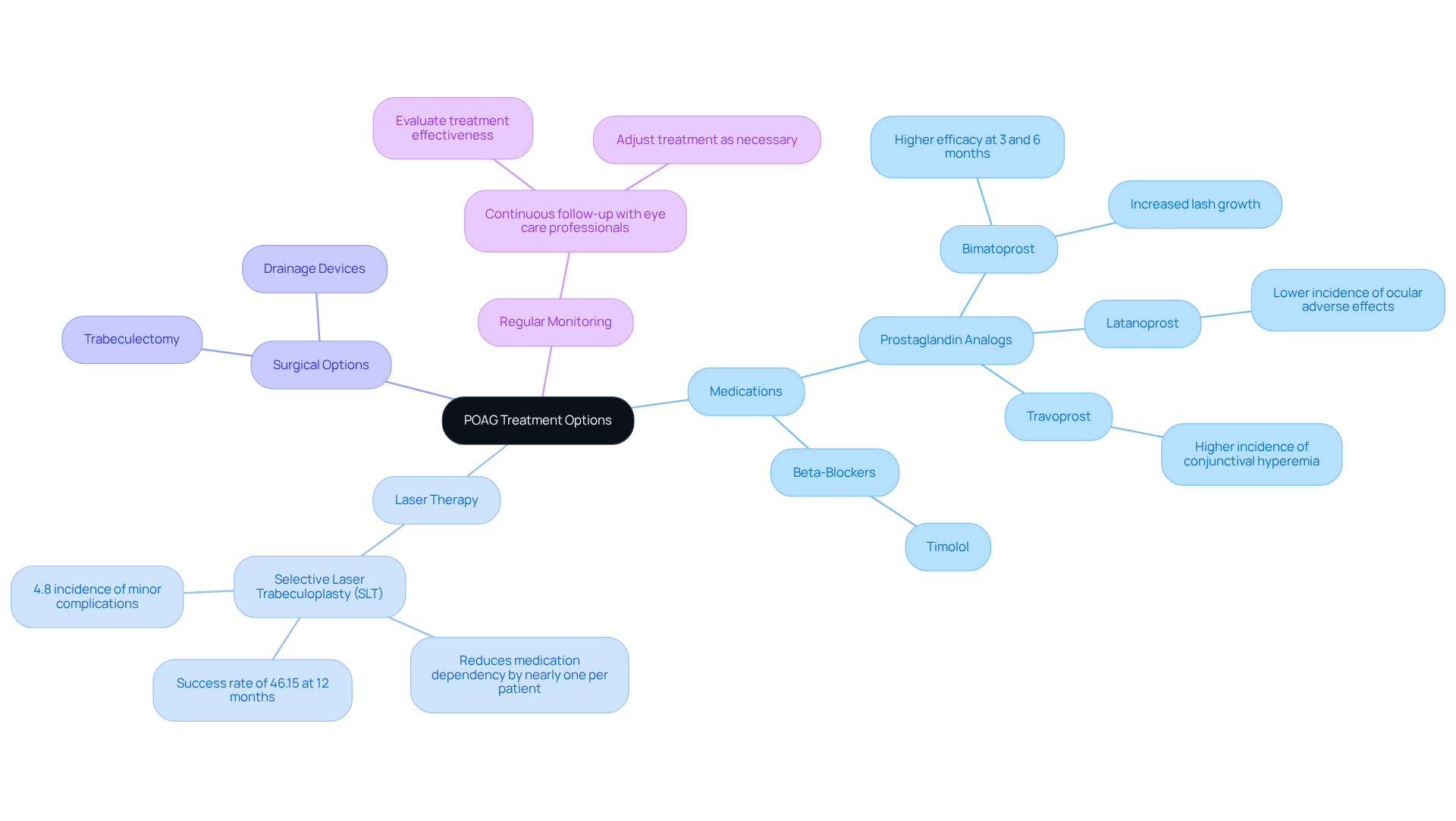
Medications are often the first step in treatment. Prescription eye drops, particularly prostaglandin analogs like latanoprost and beta-blockers such as timolol, are commonly used. These medications help by enhancing fluid drainage from your eye or reducing the production of aqueous humor, which lowers intraocular pressure (IOP). Recent studies have shown that bimatoprost, another prostaglandin analog, is particularly effective in reducing IOP compared to latanoprost and travoprost, especially at three and six months. However, it’s important to note that bimatoprost may lead to more noticeable lash growth than latanoprost.
Laser Therapy is another option worth considering. (SLT) is a minimally invasive procedure that has shown significant long-term success in lowering IOP. It works by improving fluid drainage through the trabecular meshwork. Recent data indicates that SLT can reduce the need for medications by nearly one per patient, achieving an overall success rate of about 46.15% at 12 months. Many patients find the procedure well-tolerated, with only a 4.8% incidence of minor complications, reflecting its favorable safety profile.
For those who do not achieve adequate IOP control with medications or laser therapy, surgical options may be necessary. Procedures like trabeculectomy create a new drainage pathway for fluid, while drainage devices can also be implanted. These interventions are typically considered when other treatments do not provide sufficient pressure reduction.
Regular Monitoring is crucial in this process. Continuous follow-up with your eye care professional allows for evaluating the effectiveness of the chosen treatment and making necessary adjustments. Regular assessments help ensure that your IOP remains within a target range, protecting against further optic nerve damage.
In summary, managing POAG involves a combination of medications, laser treatments, and surgical alternatives tailored to your specific needs. We are here to support you in optimizing your treatment outcomes and maintaining your eye health. Remember, you are not alone in this journey, and ongoing monitoring and care are essential for your well-being.
Examine Risk Factors for POAG
Several key risk factors contribute to the likelihood of developing POAG, and understanding these factors can empower you to take proactive steps for your eye health.
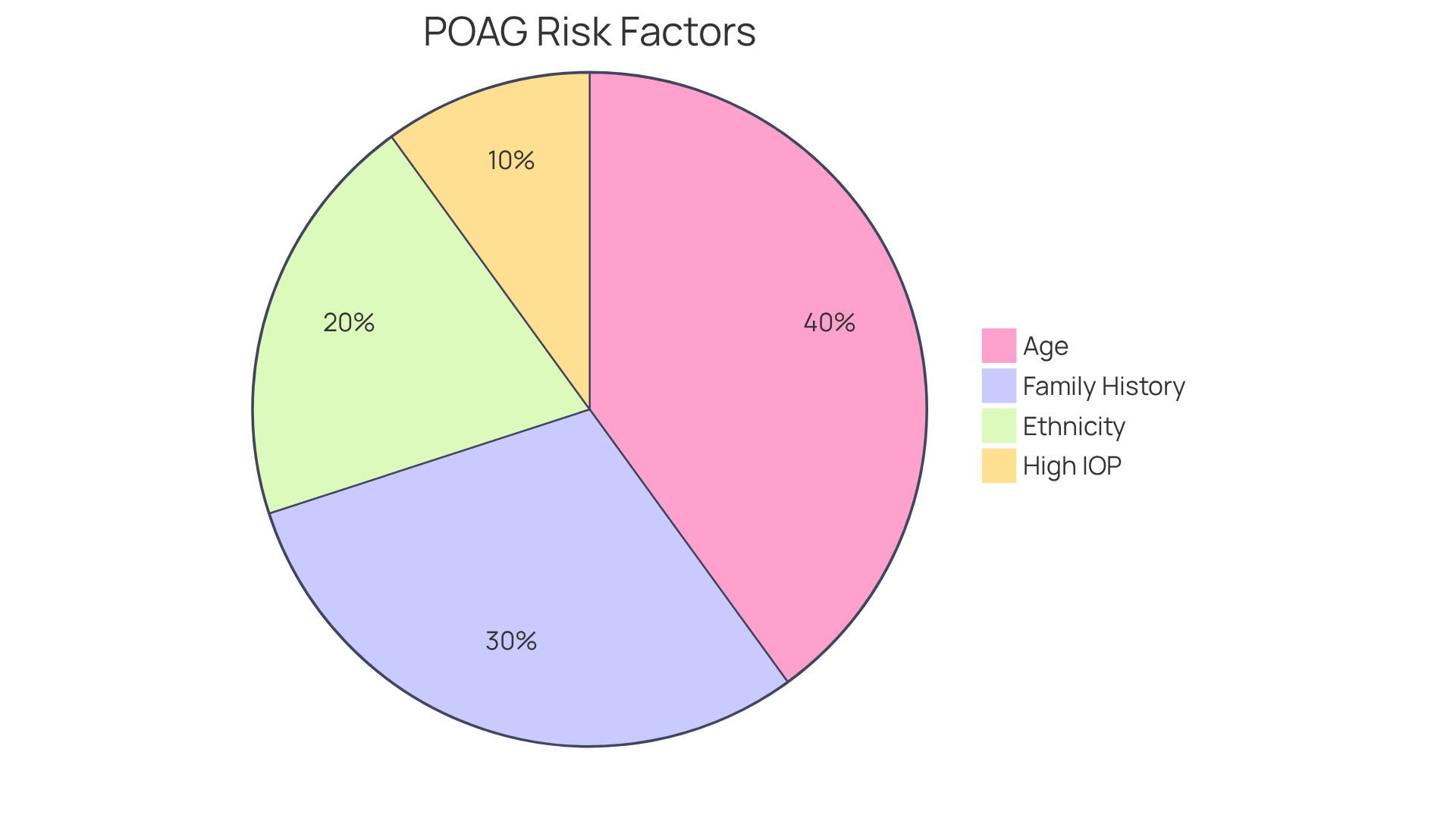
- Age: We understand that as we age, our health concerns can grow. The risk of POAG increases significantly after age 40, with a striking prevalence of POAG among individuals over 60. In fact, rates can reach up to 9.2% for those over 80.
- Family History: It’s common to feel concerned if glaucoma runs in your family. A genetic predisposition plays a crucial role; individuals with a family member diagnosed with glaucoma face an increased risk, with heritability estimates around 70%.
- Ethnicity: Certain ethnic groups, particularly African Americans, may feel more vulnerable to primary open-angle glaucoma. Prevalence rates in this demographic can reach 4.0%.
- High Intraocular Pressure (IOP): Elevated IOP is a primary risk factor for primary open-angle glaucoma. If your IOP levels are 22 mm Hg or higher, you have a seven-fold increased risk of developing the condition. Moreover, the risk increases by 0.13 times for every one mmHg increase in IOP.
It’s important to recognize that comorbidities such as diabetes, hypertension, and myopia (nearsightedness) can further elevate the risk of developing POAG.
Understanding these factors is essential for you to recognize your own risk profile. We encourage you to seek , including regular eye examinations. Remember, we are here to help you through this process.
Conclusion
Understanding Primary Open-Angle Glaucoma (POAG) is crucial for maintaining eye health and preventing irreversible vision loss. Often referred to as the “sneak thief of sight,” this condition progresses silently. We understand that being aware of its symptoms, risk factors, and treatment options is essential for early intervention and effective management.
The article highlights the significant prevalence of POAG, particularly among individuals over 40. It’s important to recognize symptoms such as:
- Gradual peripheral vision loss
- Difficulty adjusting to low light
Key risk factors include:
- Age
- Family history
- Elevated intraocular pressure
These factors can increase the likelihood of developing this condition. Furthermore, it provides an overview of treatment options, ranging from:
- Medications
- Laser therapy
- Surgical interventions
Regular monitoring and proactive eye care are vital.
In light of the alarming statistics and the potential for severe consequences if left untreated, we encourage you to prioritize your eye health. Regular eye examinations and a thorough understanding of your personal risk factors can empower you to seek timely medical advice and intervention. It’s common to feel overwhelmed, but by being proactive, you can significantly improve your chances of preserving vision and enhancing your quality of life. We are here to help you through this process.
Frequently Asked Questions
What is Primary Open-Angle Glaucoma (POAG)?
Primary Open-Angle Glaucoma (POAG) is a long-lasting eye disorder characterized by gradual damage to the optic nerve, often associated with increased intraocular pressure. It is the most common type of glaucoma and is known as the ‘sneak thief of sight’ due to its asymptomatic nature in the early stages.
How prevalent is POAG?
Approximately 2.4% of individuals over 40 years old globally are affected by primary open-angle glaucoma, with prevalence rates varying by region. For example, in Africa, the prevalence can reach up to 4.5%.
What can happen if POAG is left untreated?
If left untreated, primary open-angle glaucoma can lead to permanent vision loss and blindness, highlighting the importance of early detection and management.
What are the risk factors for developing POAG?
Risk factors for POAG include advanced age, male sex (with men having a 33% higher risk compared to women), family history of the condition, and health issues such as diabetes and hypertension.
Are there effective treatments available for POAG?
Yes, effective treatment options for POAG are available, including medications and surgical interventions that have shown promising outcomes in managing the disease and preserving vision.
How does timely treatment affect patients with POAG?
Patients who receive timely treatment often report improved visual function and a better quality of life, emphasizing the importance of proactive eye care.
What is the importance of regular visual field evaluations for POAG?
Regular visual field evaluations are essential for accurately diagnosing POAG and ensuring timely intervention, which is crucial for maintaining eye health.