Posted by: Northwest Eye in General on September 1, 2025
Overview
This article compassionately addresses the causes and solutions for the pressure you may feel behind your left eye. We understand that this sensation can be concerning, and various conditions such as migraines, sinus infections, and glaucoma can contribute to it. It’s common to feel anxious about these symptoms, but we’re here to help you navigate through this.
Regular eye exams are crucial for maintaining your vision and managing intraocular pressure effectively. Appropriate treatments, including medications, lifestyle changes, and even surgical options, can provide relief and support your eye health. Remember, you are not alone in this journey, and seeking care is a positive step towards feeling better.
We encourage you to reach out to a healthcare professional who can guide you through the available options. Your comfort and well-being are important, and together we can find the best approach to manage your symptoms and protect your vision.
Introduction
Understanding the pressure behind the left eye is crucial for maintaining optimal vision and overall eye health. We understand that this discomfort can stem from a variety of conditions, ranging from migraines to more serious issues like glaucoma. Each of these presents unique challenges and symptoms that can be concerning. As the stakes for eye health are high, recognizing the signs and seeking timely intervention can truly make all the difference.
What steps can you take to alleviate this pressure and safeguard your vision against potential threats? We are here to help you through this process.
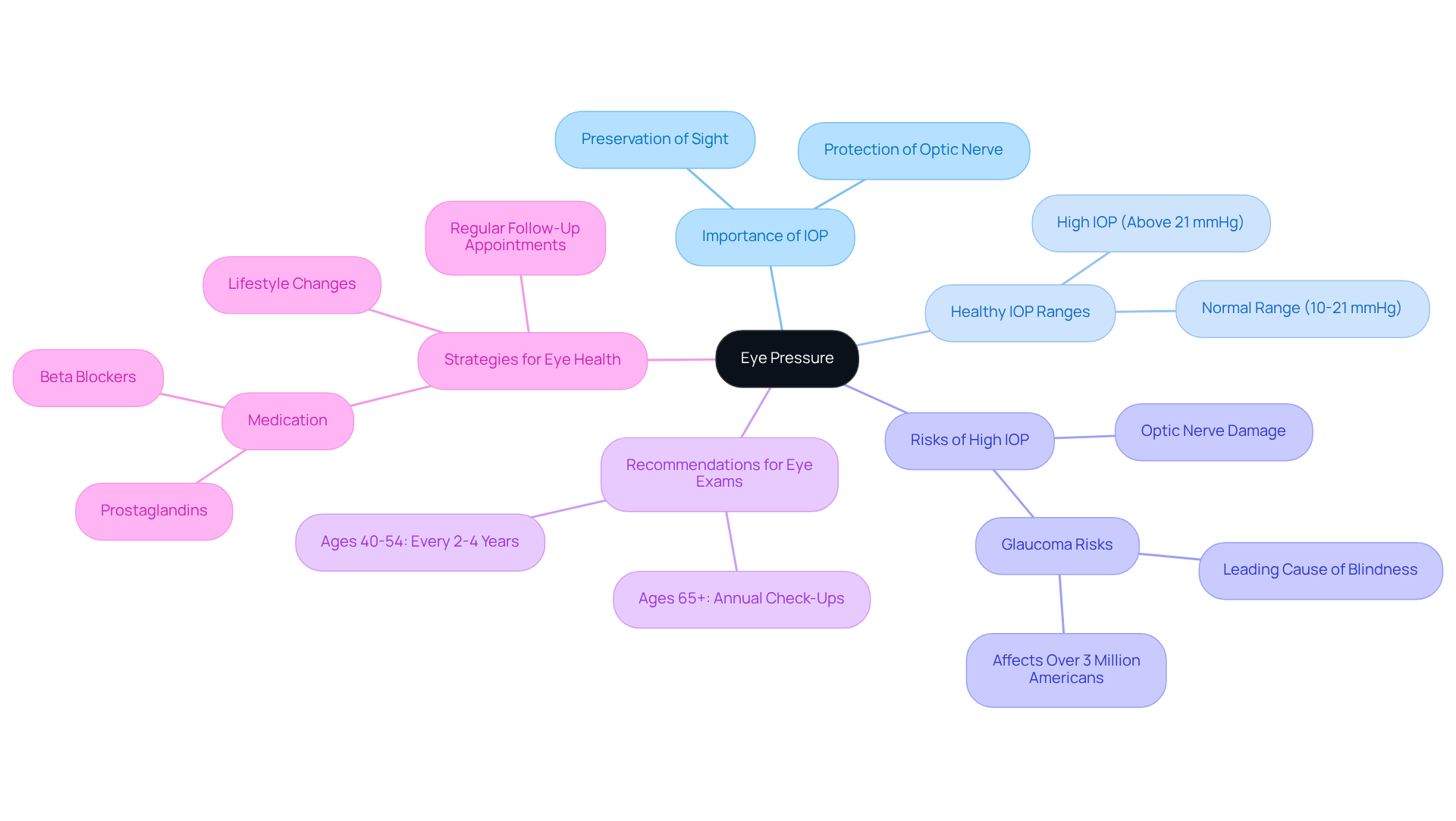
Define Eye Pressure and Its Importance
Intraocular tension (IOP) is the fluid force inside your eye, and it plays a vital role in preserving your sight and protecting the optic nerve from harm. We understand that concerns about eye health can be daunting. Healthy IOP typically ranges from 10 to 21 mmHg, with normal eye pressure generally falling between 10 mmHg and 20 mmHg. When IOP exceeds this range—especially values above 21 mmHg—the significantly increases, which can lead to irreversible vision loss. Glaucoma is a major contributor to blindness, affecting over 3 million Americans, with more than 120,000 cases resulting in total loss of sight.
It’s common to feel anxious about your eye health, but consistent monitoring of IOP is crucial for early detection and management of potential issues. Unfortunately, changes in IOP often do not present obvious symptoms until considerable damage has occurred. Research indicates that maintaining regular intraocular pressure levels is essential for safeguarding your eyesight. For instance, individuals with persistently high IOP may experience optic nerve damage, underscoring the importance of regular eye check-ups.
To ensure your eye health, expert recommendations suggest that individuals aged 40 to 54 should have comprehensive eye exams every 2 to 4 years, while those over 65 should schedule annual check-ups. The American Academy of Ophthalmology endorses these guidelines for individuals at low risk for eye disease. We are here to help you through this process.
To maintain healthy eye function, consider adopting several supportive strategies:
- Adhering to prescribed medications, such as prostaglandins and beta blockers
- Attending regular follow-up appointments
- Making lifestyle changes that promote overall eye health
Remember, you are not alone in this journey; we are dedicated to supporting you every step of the way.
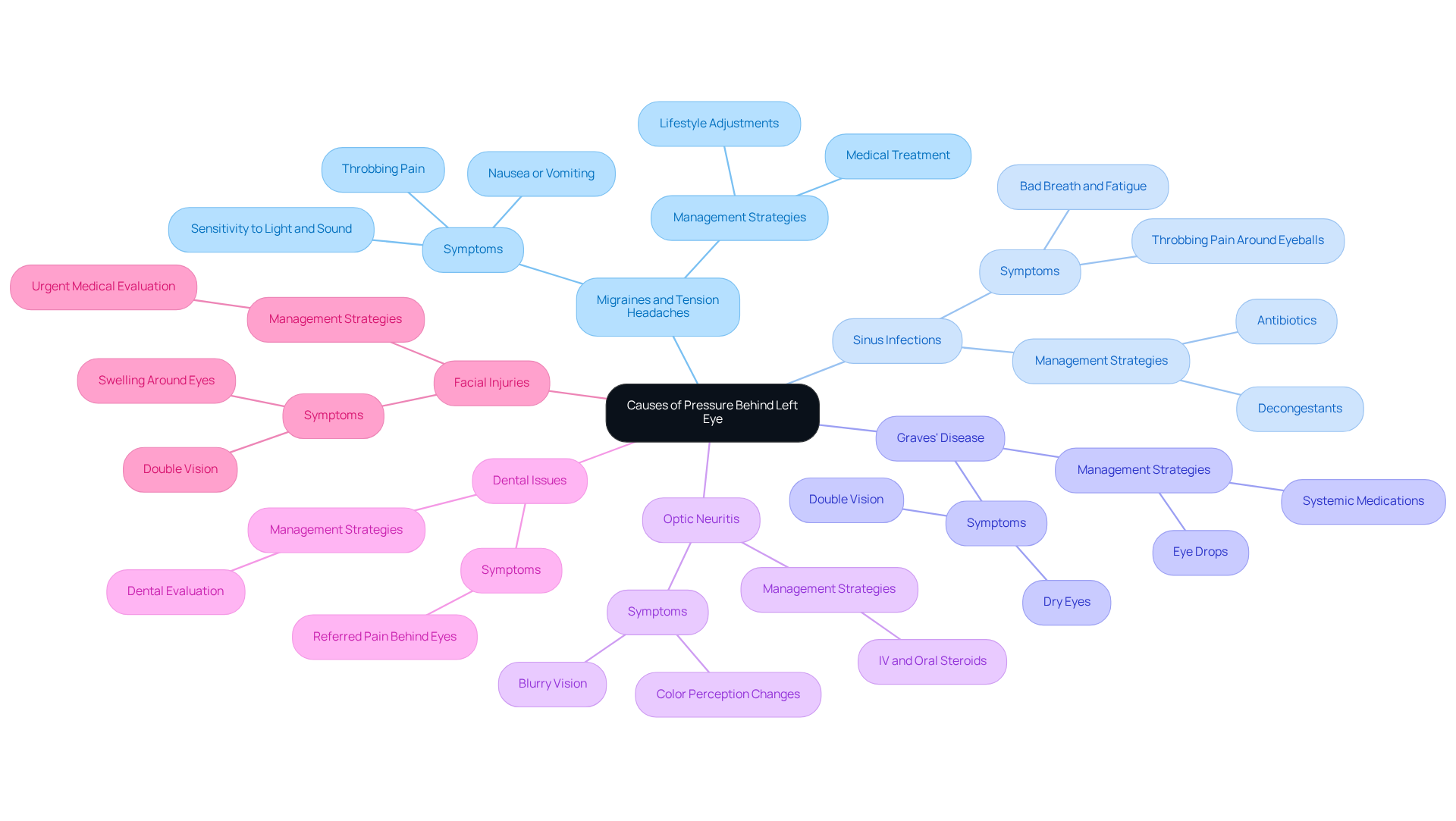
Identify Causes of Pressure Behind the Left Eye
Pressure behind left eye can arise from various conditions, each contributing to discomfort and potential vision issues. We understand that experiencing this sensation can be concerning, and it’s important to recognize the key factors that may be at play:
- Migraines and Tension Headaches: These common headache types often manifest as throbbing pain and a sensation of pressure behind the eyes. Neurologists emphasize that migraines can lead to significant discomfort, with symptoms frequently including sensitivity to light and sound. Managing headaches often involves a combination of lifestyle adjustments and medical treatment, which can bring relief.
- Sinus Infections: Inflammation of the sinus cavities can create a sensation of tension around the eyes. Sinusitis is a common cause of facial discomfort, often accompanied by symptoms like bad breath, fatigue, and headaches. It’s common to feel overwhelmed by these symptoms, but untreated sinus infections can lead to serious complications, including eye problems. One of the primary symptoms of a sinus infection is throbbing pain and discomfort around the eyeballs, so seeking care is essential.
- Graves’ Disease: This autoimmune condition can lead to inflammation of the tissues located behind the orbs, resulting in a feeling of tension. Symptoms may include dry eyes and double vision, highlighting the importance of medical evaluation for those experiencing these issues. The swelling of the tissues behind the eye may lead to a sensation of tightness, and we encourage anyone facing these symptoms to consult a healthcare professional.
- Optic Neuritis: Inflammation of the optic nerve can lead to pain and pressure behind the affected eye, often associated with conditions like multiple sclerosis. Symptoms generally encompass unclear sight and alterations in color perception, necessitating swift medical care. If you notice reduced vision or changes in color perception, it’s important to seek help promptly.
- Dental Issues: Tooth infections or alignment problems can result in referred pain, causing feelings of discomfort behind the orbs. This connection underscores the need for dental evaluations when experiencing unexplained eye discomfort. If you suspect tooth alignment issues, consulting a dentist for a thorough examination can be a crucial step toward relief.
- Facial Injuries: Trauma to the face, including fractures or muscle damage, can lead to swelling and discomfort around the eyes. Symptoms may consist of double sight and facial numbness, necessitating urgent medical evaluation to avoid additional complications. Recognizing these warning signs can lead to timely medical intervention, ensuring that underlying issues are addressed appropriately.
Comprehending these underlying factors is essential for effective management and alleviation of the pressure behind left eye. Regular check-ups with healthcare professionals, including comprehensive eye exams and dental evaluations, can aid in identifying and addressing these issues promptly. We encourage you to seek immediate care for sudden, with alarming symptoms, as they may indicate serious underlying conditions. Remember, we are here to help you through this process.
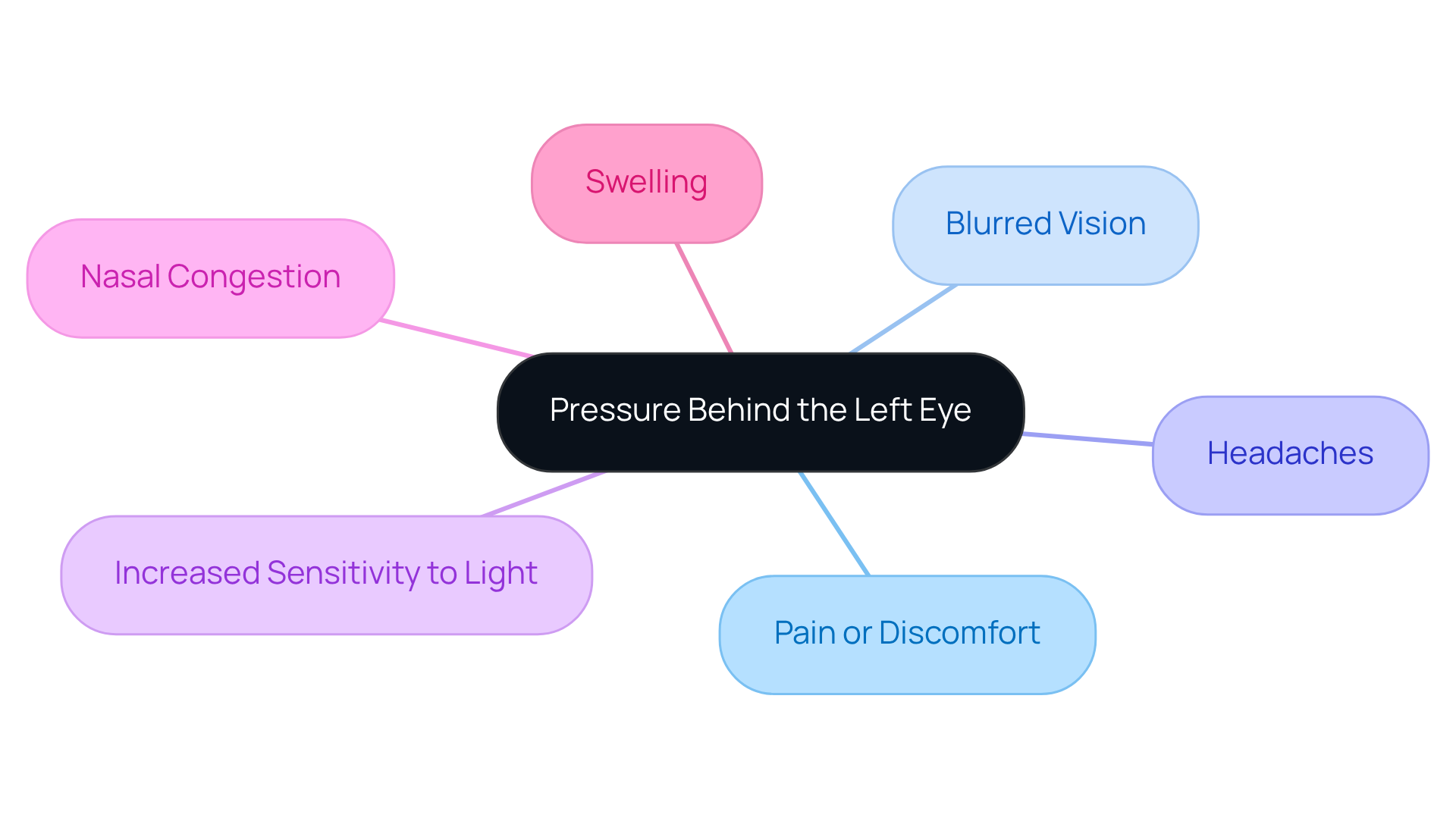
Recognize Symptoms of Pressure Behind the Left Eye
Symptoms related to the can manifest in various ways, significantly affecting your comfort and vision. We understand that experiencing these symptoms can be distressing, and it’s important to recognize them. Common indicators include:
- Pain or Discomfort: Many patients report a sensation of fullness or aching behind the eye, which can be quite uncomfortable.
- Blurred vision may make it difficult to focus, often accompanied by a feeling of tightness and pressure behind the left eye, which makes clear vision a challenge.
- Headaches can occur alongside the pressure behind the left eye and vary in intensity, adding to your overall discomfort.
- Increased sensitivity to light may occur, which can complicate your visual comfort and is often associated with the pressure behind the left eye.
- Nasal congestion can arise, especially if sinus issues are contributing to the pressure behind the left eye and your discomfort.
- Swelling: In some cases, you may notice visible swelling around the eye area, which can be a sign of pressure behind the left eye and indicate potential underlying issues.
Increased intraocular tension is a significant concern, as it can lead to optic nerve injury and loss of sight if not properly addressed. It’s common to feel anxious about symptoms like blurred vision and discomfort; however, it’s crucial to seek immediate medical evaluation. Conditions such as glaucoma can develop silently, often without noticeable symptoms until they reach advanced stages. Regular eye exams are essential for early detection and management of these issues, ensuring you maintain optimal eye health. Remember, we are here to help you through this process and ensure you receive the care you need.
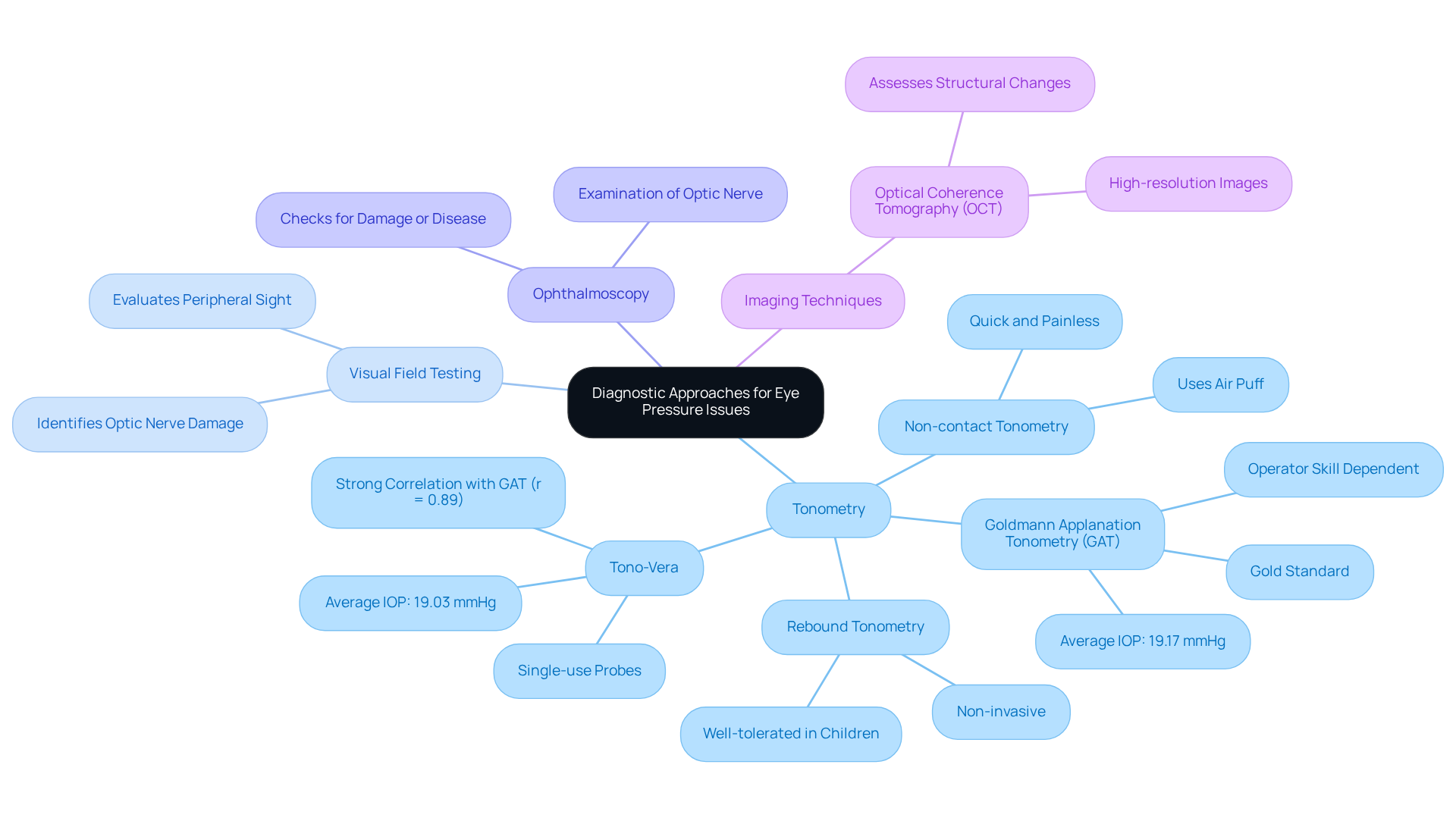
Explore Diagnostic Approaches for Eye Pressure Issues
We understand that feeling pressure behind the left eye can be concerning. Diagnosing these issues typically involves several compassionate approaches:
- Tonometry: This essential test measures intraocular pressure (IOP) using various methods. Goldmann applanation tonometry (GAT) is considered the gold standard, providing accurate readings by flattening the cornea with a disk-shaped extension. The average IOP for the population measured by GAT was found to be 19.17 mmHg, while Tono-Vera recorded an average of 19.03 mmHg, demonstrating a strong correlation (r = 0.89) between the two methods. Other methods include non-contact tonometry, which uses a puff of air to assess pressure, and rebound tonometry, which employs a small plastic ball that gently contacts the eye. Each method offers unique advantages, with GAT being particularly reliable but dependent on operator skill. Notably, rebound tonometry is non-invasive and well-tolerated, making it suitable for pediatric patients.
- Visual Field Testing: This assessment evaluates peripheral sight and can reveal damage to the optic nerve, which is often associated with elevated IOP and the pressure behind the left eye. By mapping the visual field, eye care specialists can identify areas of vision loss that may indicate underlying conditions such as glaucoma. We know that routine follow-up appointments are crucial if ocular tension is elevated, guaranteeing continuous care of your eye health.
- Ophthalmoscopy: A thorough examination of the optic nerve and retina is conducted to check for signs of damage or disease. This technique enables experts to observe the condition of the optic nerve head, which can be influenced by the pressure behind the left eye.
- Imaging Techniques: Advanced imaging modalities, such as Optical Coherence Tomography (OCT), provide high-resolution images of the optic nerve and retina. These images help in assessing structural changes that may occur due to elevated IOP, enabling timely intervention. During applanation tonometry, anesthetic eye drops may be used, which can cause temporary discomfort; we want you to be informed about this aspect of the procedure.
Together, these create a comprehensive strategy for assessing eye tension concerns, ensuring that you receive precise evaluations and suitable care. Remember, we are here to help you through this process.
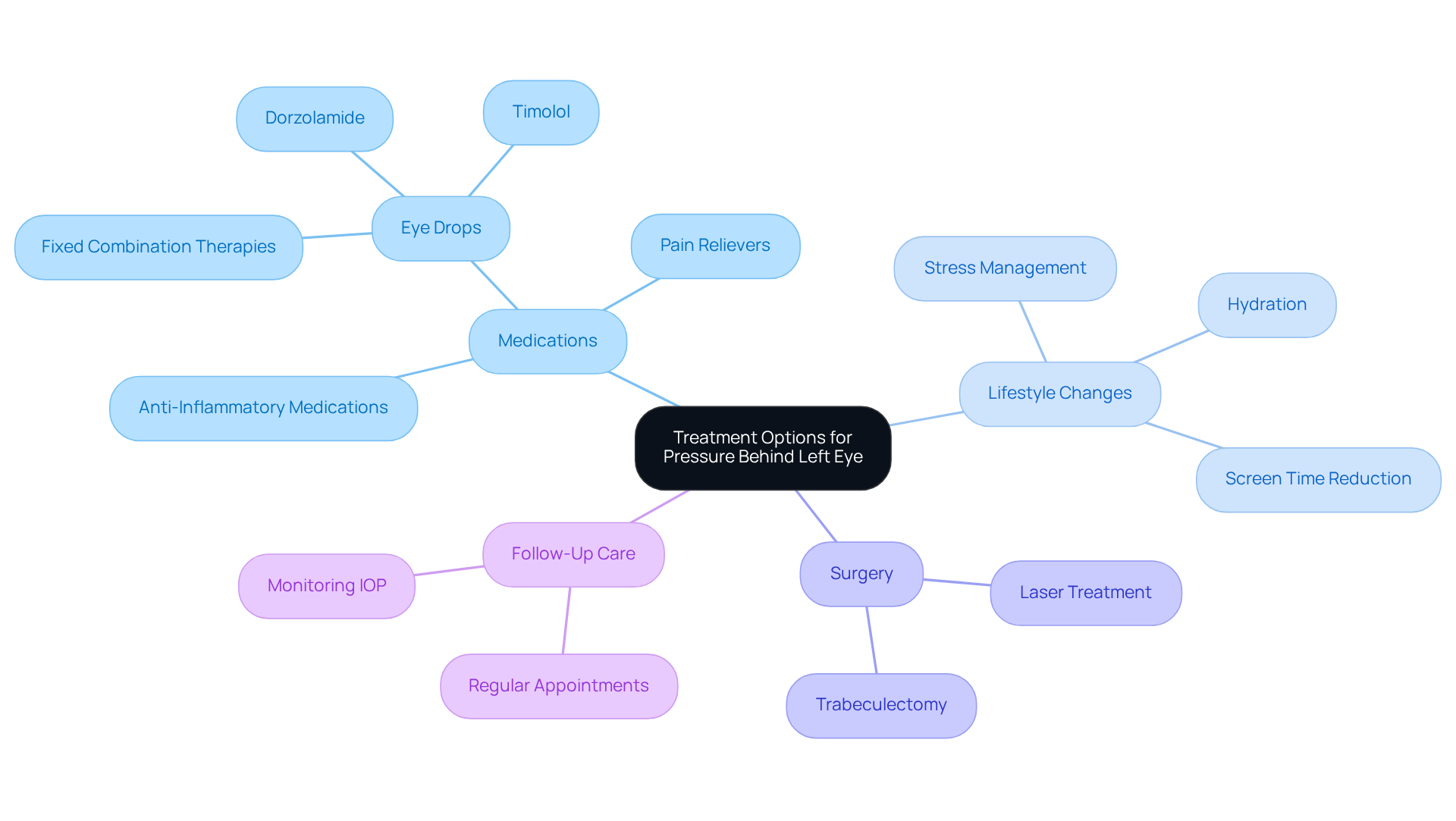
Review Treatment Options for Pressure Behind the Left Eye
Managing the pressure behind the left eye can feel overwhelming, but we are here to help you through this process. It involves a multifaceted approach that includes medications, lifestyle changes, surgical interventions, and diligent follow-up care.
- Medications: Prescription eye drops are often used to help reduce intraocular tension (IOP). These might include fixed combination therapies, which have shown superior efficacy in lowering IOP compared to non-fixed combinations. For example, studies indicate that fixed combination dorzolamide/timolol maleate can achieve a peak IOP reduction of approximately 32.7% and a sustained reduction of 27%. Additionally, dorzolamide alone can reduce IOP by 17%-32%, while timolol can lower it by 20%-28%. Pain relievers and anti-inflammatory medications may also be prescribed to alleviate discomfort linked to increased eye tension.
- Lifestyle Changes: We understand that implementing lifestyle modifications can significantly impact IOP management. Stress management techniques, staying adequately hydrated, and minimizing triggers such as excessive screen time are recommended. Research highlights that adhering to these changes can enhance treatment outcomes, as patients who actively engage in their care often experience better IOP control. For instance, one patient shared that by managing stress and maintaining hydration, they observed a significant improvement in their eye measurements.
- Surgery: In some cases, where glaucoma or other conditions lead to significant tension, surgical options may be necessary. Methods like laser treatment or trabeculectomy can effectively lower eye tension and prevent further sight deterioration. These interventions are typically considered when medications and lifestyle adjustments are not enough. Studies show that surgical options can lead to significant long-term improvements in IOP management.
- Follow-Up Care: Regular follow-up appointments are crucial for monitoring IOP and adjusting treatment plans as needed. We know that help ensure any fluctuations in ocular tension are swiftly managed, enhancing patient outcomes. Adherence to follow-up care has been shown to significantly impact treatment efficacy, with studies indicating that patients who maintain regular appointments experience better control of their IOP.
In summary, effective management for pressure behind left eye involves a combination of medications, lifestyle adjustments, surgical options, and ongoing care. Our ultimate goal is to preserve your vision and enhance your quality of life.
Conclusion
Understanding the pressure behind the left eye is crucial for maintaining optimal eye health and preventing potential vision loss. We recognize that this can be a source of concern for many, and it’s important to highlight the significance of intraocular pressure (IOP) and its relationship to various medical conditions. Regular eye examinations and timely interventions are essential, and we encourage you to prioritize these for your well-being.
There are diverse factors that contribute to pressure behind the left eye, such as:
- Migraines
- Sinus infections
- Graves’ disease
- More
Each condition presents unique symptoms that warrant medical attention. It’s common to feel overwhelmed by this information, but remember that diagnostic approaches like tonometry and visual field testing are essential tools for healthcare professionals to assess and manage eye pressure effectively.
Treatment options, ranging from medications to surgical interventions, underscore the importance of a comprehensive management strategy tailored to your individual needs. We want you to feel reassured that there are effective ways to address these concerns.
Ultimately, maintaining awareness of eye pressure and its implications is vital for everyone. Regular check-ups, lifestyle modifications, and adherence to prescribed treatments can significantly improve outcomes and enhance your quality of life. By prioritizing your eye health and seeking timely care, you can protect your vision and ensure long-term well-being. We are here to help you through this process, and we encourage you to take proactive steps towards safeguarding your vision.
Frequently Asked Questions
What is intraocular pressure (IOP) and why is it important?
Intraocular pressure (IOP) is the fluid force inside your eye, crucial for preserving sight and protecting the optic nerve. Healthy IOP typically ranges from 10 to 21 mmHg, with normal levels between 10 mmHg and 20 mmHg. Elevated IOP, particularly above 21 mmHg, increases the risk of developing glaucoma, which can lead to irreversible vision loss.
How often should I have my eye pressure checked?
Individuals aged 40 to 54 should have comprehensive eye exams every 2 to 4 years, while those over 65 should schedule annual check-ups. These recommendations are endorsed by the American Academy of Ophthalmology for individuals at low risk for eye disease.
What are some strategies to maintain healthy eye function?
To maintain healthy eye function, consider adhering to prescribed medications, attending regular follow-up appointments, and making lifestyle changes that promote overall eye health.
What could cause pressure behind the left eye?
Pressure behind the left eye can result from several conditions, including migraines, sinus infections, Graves’ disease, optic neuritis, dental issues, and facial injuries.
How do migraines contribute to pressure behind the eye?
Migraines can cause throbbing pain and a sensation of pressure behind the eyes, often accompanied by sensitivity to light and sound. Managing migraines typically involves lifestyle adjustments and medical treatment.
What are the symptoms of a sinus infection related to eye pressure?
A sinus infection can lead to inflammation of the sinus cavities, resulting in discomfort around the eyes, bad breath, fatigue, and headaches. It can cause throbbing pain and discomfort around the eyeballs.
What is Graves’ disease and how does it affect eye pressure?
Graves’ disease is an autoimmune condition that can cause inflammation of the tissues behind the eyes, leading to a sensation of tension. Symptoms may include dry eyes and double vision, necessitating medical evaluation.
What is optic neuritis, and what symptoms should I look out for?
Optic neuritis is inflammation of the optic nerve that can cause pain and pressure behind the affected eye. Symptoms may include unclear vision and changes in color perception, requiring prompt medical attention.
How can dental issues cause discomfort behind the eyes?
Tooth infections or alignment problems can lead to referred pain, causing discomfort behind the eyes. It is important to seek dental evaluations when experiencing unexplained eye discomfort.
When should I seek immediate medical care for eye pressure concerns?
You should seek immediate medical care for sudden, severe headaches accompanied by alarming symptoms, as they may indicate serious underlying conditions. Regular check-ups with healthcare professionals can help identify and address issues promptly.