Posted by: Northwest Eye in General on August 14, 2025
Overview
Retinal detachment occurs when the retina pulls away from its normal position, which can be a distressing experience. We understand that this poses a serious risk of permanent vision loss if not treated promptly. This article outlines the causes, symptoms, and various effective treatment options available. It emphasizes the importance of early detection and medical intervention, which can significantly enhance patient outcomes and help preserve vision.
Remember, you are not alone in this journey; we are here to help you through this process.
Introduction
Retinal detachment is a critical eye condition that can lead to irreversible vision loss if not addressed swiftly. We understand that this alarming reality affects approximately 1 in 10,000 individuals annually, which makes awareness of its causes, symptoms, and treatment options essential for maintaining eye health.
How can you recognize the early signs of this condition, and what proactive steps can you take to mitigate the risks? Understanding these factors is vital for anyone seeking to safeguard their vision and navigate the complexities of retinal health. We are here to help you through this process.
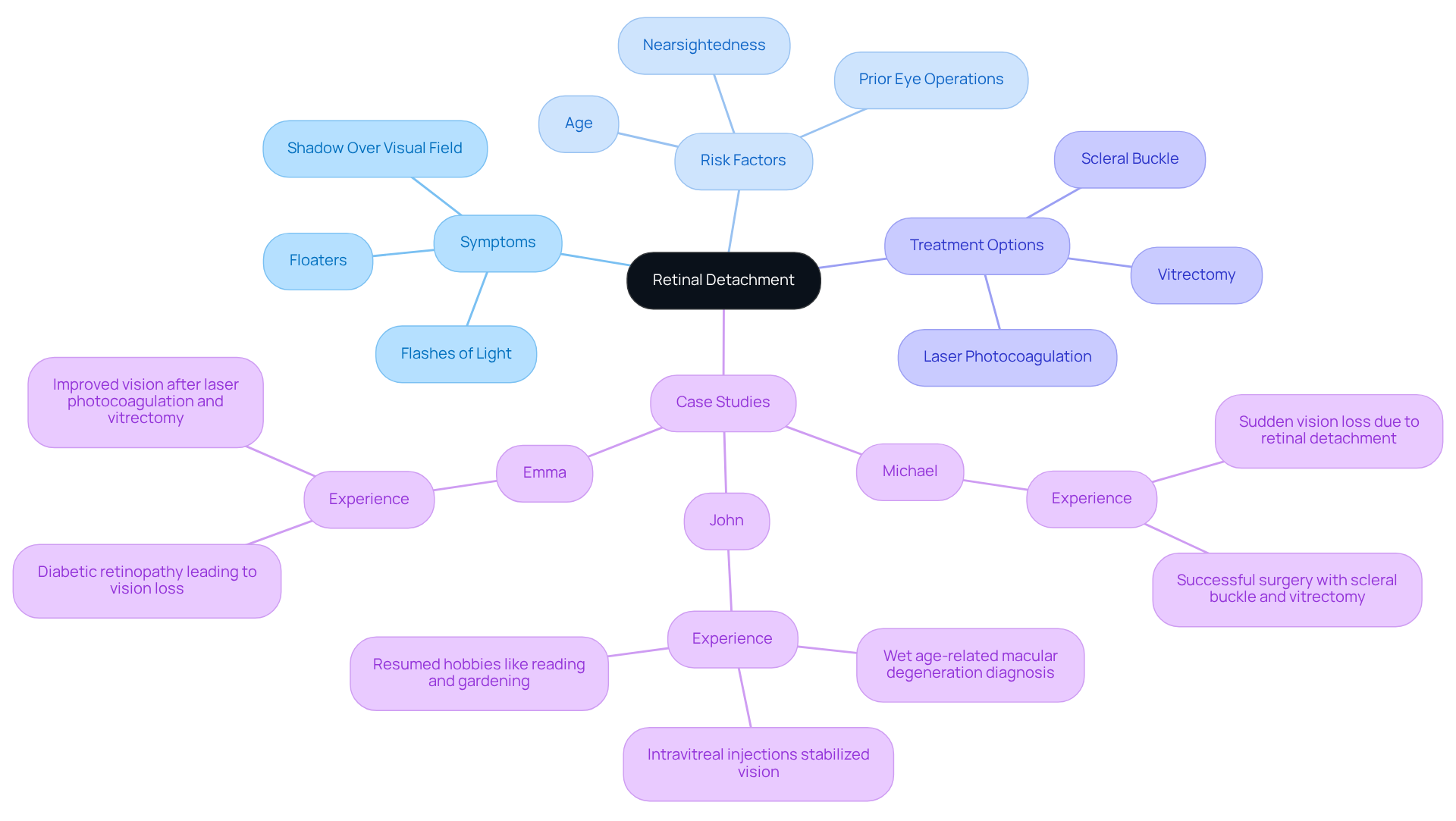
Define Retinal Detachment: Importance and Overview
occurs when the retina, which is a thin layer of tissue at the back of the eye, pulls away from its normal position. We understand that this condition can be alarming, as it may lead to if not treated promptly. This makes it a medical emergency due to the potential for irreversible damage to the retina caused by retina detachment, which is essential for vision. Grasping this condition is crucial for early identification and action, greatly enhancing outcomes for individuals showing signs of eye separation.
Understanding eye separation is essential, as it impacts roughly 1 in 10,000 people each year. :
- Sudden flashes of light
- Floaters
- A shadow over the visual field
It’s common to feel anxious about these symptoms, but recent studies suggest that . Many individuals recover considerable sight after surgical procedures. For example, Michael, a 55-year-old enthusiastic golfer, suffered abrupt vision loss due to a retinal separation but had successful surgery involving a and vitrectomy. He shared, ‘I was terrified when I lost my sight, but the surgery changed everything for me.’
Elements like age, nearsightedness, and prior eye operations can elevate the risk of developing retina detachment. We emphasize the importance of , especially for those at higher risk, to facilitate early detection and treatment. Taking proactive steps can make a difference in your eye health.
Case studies further illustrate the impact of retina detachment on individuals’ lives. For instance, John, a 68-year-old retired teacher diagnosed with wet age-related macular degeneration, underwent intravitreal injections that stabilized his sight, enabling him to return to his hobbies. Similarly, Emma, a 40-year-old with diabetes, faced vision loss due to diabetic retinopathy but improved significantly after laser photocoagulation and vitrectomy. These narratives highlight the resilience of patients and the effectiveness of in managing eye conditions. We are here to help you through this process, ensuring that you receive the care you need.
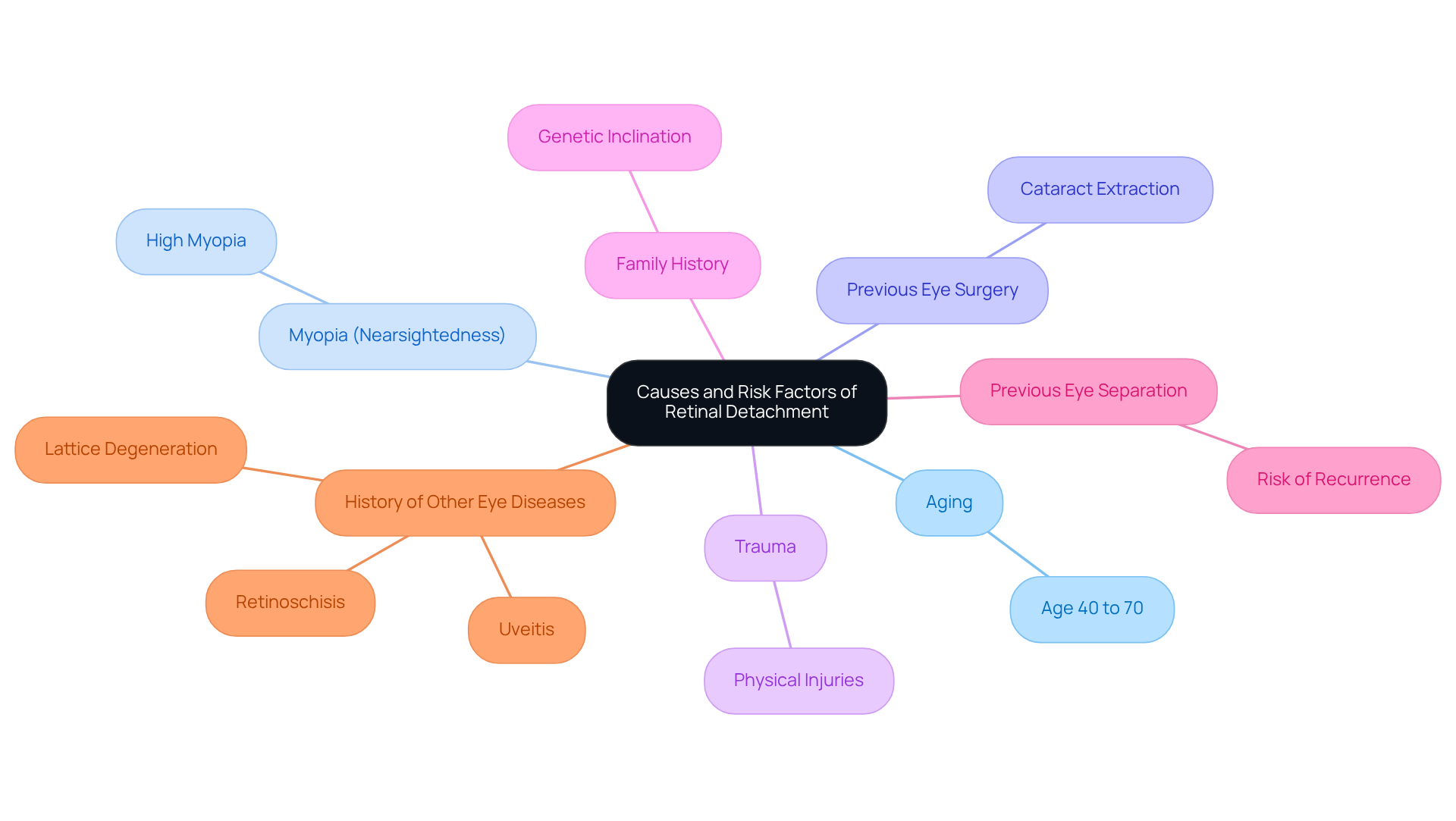
Explore Causes and Risk Factors of Retinal Detachment
can arise from several key , with each factor contributing to the likelihood of this serious condition. We understand that learning about these risks can be concerning, but knowledge is the first step towards proactive care.
- Aging: The risk escalates significantly for individuals aged 40 to 70, as age-related changes in the eye can lead to detachment.
- (Nearsightedness): Those with high myopia face an increased risk of retina detachment due to the elongation of the eyeball, which can create tension on the retina and lead to tears.
- Previous Eye Surgery: Surgeries, especially cataract extraction, can increase the likelihood of separation of the retina due to changes in the eye’s structure.
- Trauma: Physical injuries to the eye can result in retina detachment, requiring urgent medical attention.
- Family History: A genetic inclination plays a significant role; individuals with a are at a higher risk.
- Previous Eye Separation: Individuals who have undergone eye separation in one eye are at a heightened risk of it happening in the other eye.
- History of Other : Conditions such as retinoschisis, uveitis, or lattice degeneration can also increase the risk of retina detachment.
Recognizing these risk factors is crucial for early detection and implementing effective prevention strategies. It’s common to feel uncertain if you notice new floaters or alterations in your sight. We encourage you to seek a quickly, as these symptoms can suggest possible eye problems. As Amir Khan, M.D. states, “In the back of our eyes, we have a substance called ‘the vitreous.’ When we’re young, it’s a firm clump of jelly. As we age, this firm clump of jelly can liquefy and break up into smaller pieces. Those smaller pieces are what you may notice as floaters.” This highlights the significance of observing alterations in vision, as can indicate underlying issues that may lead to retina detachment.
Retina detachment is an in which the from its usual position, making essential. We are here to help you through this process, ensuring you receive the care and support you need.
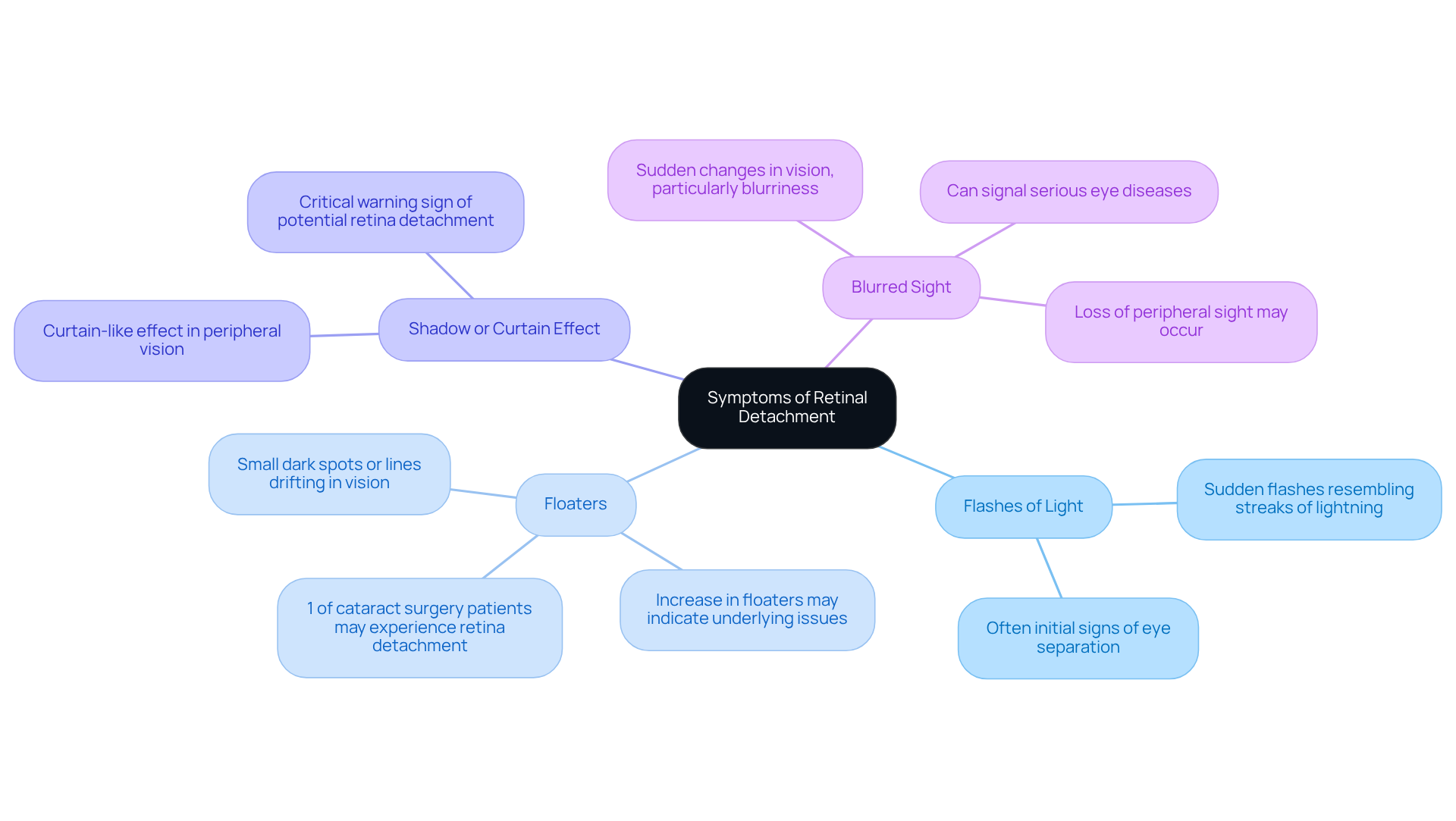
Identify Symptoms of Retinal Detachment
Indicators of eye separation can manifest in various ways, often serving as critical alerts for the need for medical care. We understand that noticing changes in your vision can be concerning, and it’s important to be aware of the key indicators, which include:
- Flashes of Light: You might experience , resembling streaks of lightning, in one or both eyes. These are often among the of eye separation, and we want you to feel reassured.
- Floaters: An —small dark spots or lines drifting across your field of vision—can indicate underlying issues. It’s worth noting that approximately one percent of patients who have undergone may experience , typically marked by a . Knowing this can help you understand that you are not alone in your experience.
- : If you notice a shadow or curtain-like effect in your peripheral vision, this is a critical warning sign that suggests there may be retina detachment. This symptom can lead to significant loss of sight if not addressed promptly, and we encourage you to take it seriously.
- : Sudden changes in your vision, particularly blurriness, can indicate retina detachment. Blurred sight may arise from various conditions, including cataracts, diabetic retinopathy, and uncorrected refractive errors, and it can signal serious eye diseases. Additionally, loss of peripheral sight may occur, further highlighting the importance of seeking consultation with an ophthalmologist.
Identifying these signs promptly is crucial, as can help avert permanent sight loss. Remember, retina detachment is painless, which can make it even more insidious. If you experience any of these signs, we urge you to seek immediate medical attention to safeguard your vision. We are here to help you through this process.
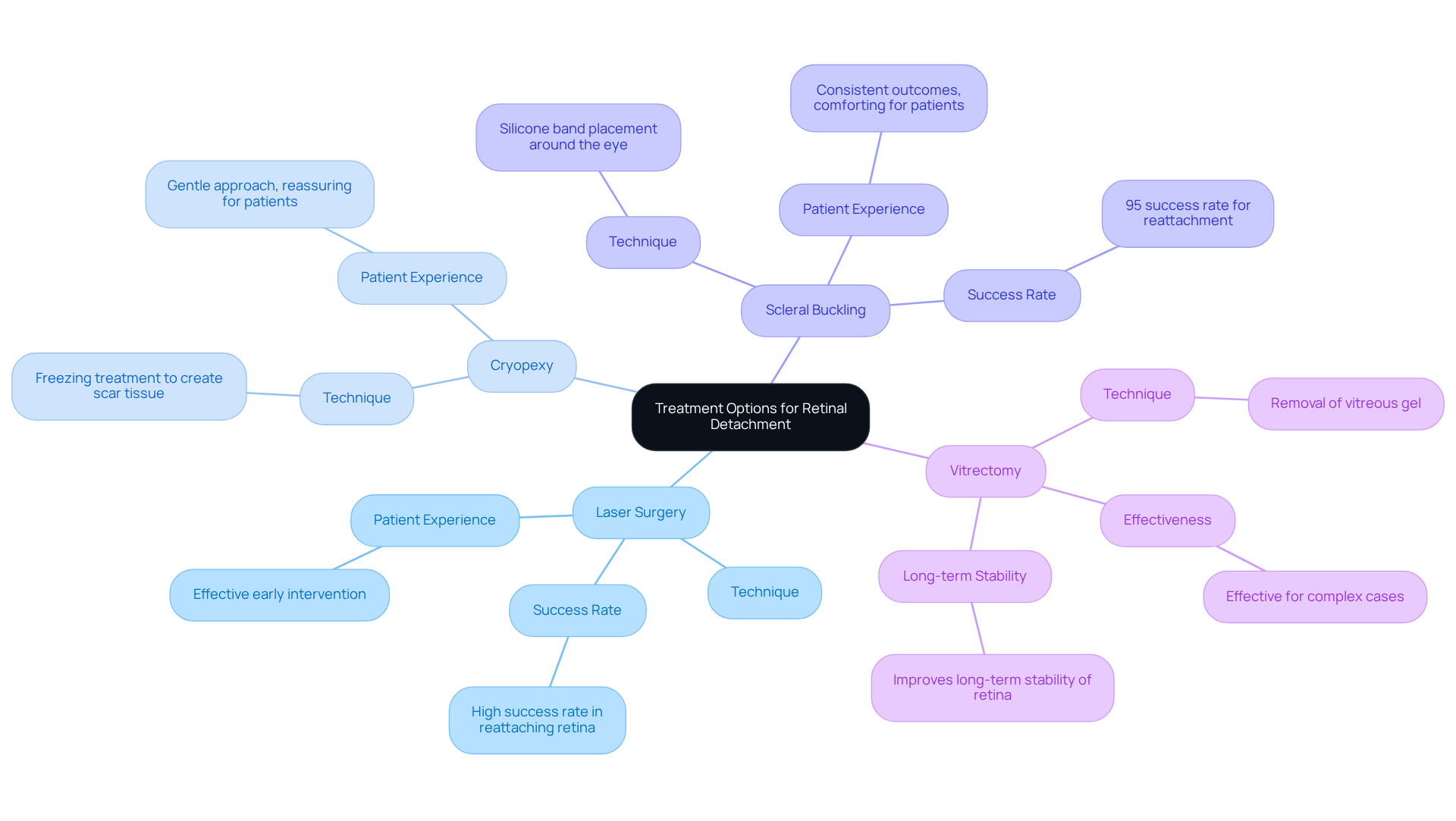
Review Treatment Options for Retinal Detachment
We understand that facing can be a daunting experience. It’s common to feel anxious about what lies ahead, but rest assured, there are several available to help you regain your vision.
- (Photocoagulation): This technique uses lasers to seal retinal tears, effectively preventing further detachment. Many studies show that laser surgery achieves a high in reattaching the retina after a retina detachment, making it a vital option for .
- : This freezing treatment assists in reattaching the retina by creating scar tissue around the tear, providing a stable environment for healing. It’s a gentle approach that many patients find reassuring.
- : In this procedure, a silicone band is placed around the eye to gently push the wall of the eye against the retina, facilitating reattachment. Scleral buckling has shown consistent outcomes, with for addressing retina detachment, especially when performed promptly. It’s comforting to know that repair for retina detachment has a similar success rate, reinforcing the effectiveness of this treatment.
- Vitrectomy: This involves removing the vitreous gel that may be exerting traction on the retina, allowing it to settle back into its proper position. Vitrectomy is particularly effective for complex cases, as it can help prevent retina detachment, leading to improved long-term stability of the retina post-surgery.
Each treatment option is tailored to your specific circumstances, and early intervention is crucial for preserving your vision. The advancements in these surgical techniques have significantly enhanced patient outcomes, with many individuals returning to their normal activities within a week after surgery. According to recent data, 91% of patients in the per-protocol group experienced successful reattachment, highlighting the effectiveness of these interventions. We are here to help you through this process and ensure you receive the care you need.
Conclusion
Understanding retinal detachment is crucial, as it poses a significant risk to your vision if not addressed promptly. This serious condition, characterized by the separation of the retina from its underlying tissue, can lead to irreversible damage and permanent vision loss. We understand that recognizing the urgency of this medical emergency can be overwhelming, but taking swift action can significantly improve your chances of recovery.
In this article, we delve into the various aspects of retinal detachment, including its causes, symptoms, and treatment options. Key risk factors such as:
- Aging
- Nearsightedness
- Previous eye surgeries
highlight the importance of regular eye examinations for early detection. Symptoms like:
- Flashes of light
- Floaters
- Blurred vision
serve as vital warning signs, urging you to seek immediate medical attention. Moreover, our discussion on treatment options, including:
- Laser surgery
- Vitrectomy
underscores the advancements in eye care that can restore sight and improve outcomes for patients like you.
Ultimately, awareness and education about retinal detachment are essential for safeguarding your vision. We encourage you to monitor your eye health closely and seek prompt medical advice upon noticing any concerning symptoms. By prioritizing your eye health and understanding the implications of retinal detachment, you can take proactive steps towards preserving your vision and enhancing your overall well-being. Remember, we are here to help you through this process.
Frequently Asked Questions
What is retinal detachment?
Retinal detachment occurs when the retina, a thin layer of tissue at the back of the eye, pulls away from its normal position. It is a medical emergency that can lead to permanent vision loss if not treated promptly.
Why is retinal detachment considered a medical emergency?
It is considered a medical emergency because if not treated quickly, retinal detachment can cause irreversible damage to the retina, which is essential for vision.
What are the common symptoms of retinal detachment?
Common symptoms include sudden flashes of light, floaters, and a shadow over the visual field.
How prevalent is retinal detachment?
Retinal detachment impacts roughly 1 in 10,000 people each year.
Can treatment improve outcomes for retinal detachment?
Yes, prompt treatment can significantly improve patient outcomes, and many individuals recover considerable sight after surgical procedures.
What are some risk factors for developing retinal detachment?
Risk factors include age, nearsightedness, and prior eye operations.
How important are regular eye examinations for those at risk?
Regular eye examinations are crucial for early detection and treatment of retinal detachment, especially for individuals at higher risk.
Can you provide examples of individuals who have successfully managed retinal detachment?
Yes, for instance, Michael, a 55-year-old golfer, had successful surgery after sudden vision loss due to retinal separation. Similarly, John, a 68-year-old retired teacher, stabilized his sight with intravitreal injections, and Emma, a 40-year-old with diabetes, improved significantly after laser photocoagulation and vitrectomy.
What types of surgeries are commonly performed for retinal detachment?
Common surgical procedures include scleral buckle, vitrectomy, and laser photocoagulation.