Posted by: Northwest Eye in General on August 15, 2025
Overview
Cystoid macular edema (CME) can be a concerning condition, primarily caused by fluid accumulation in the macula. This may occur due to various factors, such as:
- post-surgical inflammation
- diabetes
- uveitis
- retinal vein occlusion
We understand that the prospect of significant visual impairment can be distressing.
Timely diagnosis and treatment are crucial for managing CME and preventing potential vision loss. Effective options include:
- anti-inflammatory medications
- anti-VEGF therapy
It’s common to feel overwhelmed, but knowing the causes and symptoms of CME can empower you in your journey towards effective care.
We are here to help you through this process. Understanding the importance of seeking timely treatment can make a significant difference in your visual health. Remember, you are not alone in this; support and reassurance are available to guide you.
Introduction
Cystoid macular edema (CME) is a condition that understandably raises concern due to its potential to disrupt central vision, which is so vital to our daily lives. With fluid accumulation leading to swelling in the macula, it is essential to understand the causes, symptoms, and treatment options for CME in order to maintain visual health.
It’s common to feel anxious about what happens when this seemingly manageable condition escalates into a significant threat to sight, especially following common procedures like cataract surgery.
Exploring the intricacies of CME not only reveals its impact on individuals but also highlights the urgent need for timely diagnosis and effective management strategies. We are here to help you through this process.
Define Cystoid Macular Edema: Key Concepts and Terminology
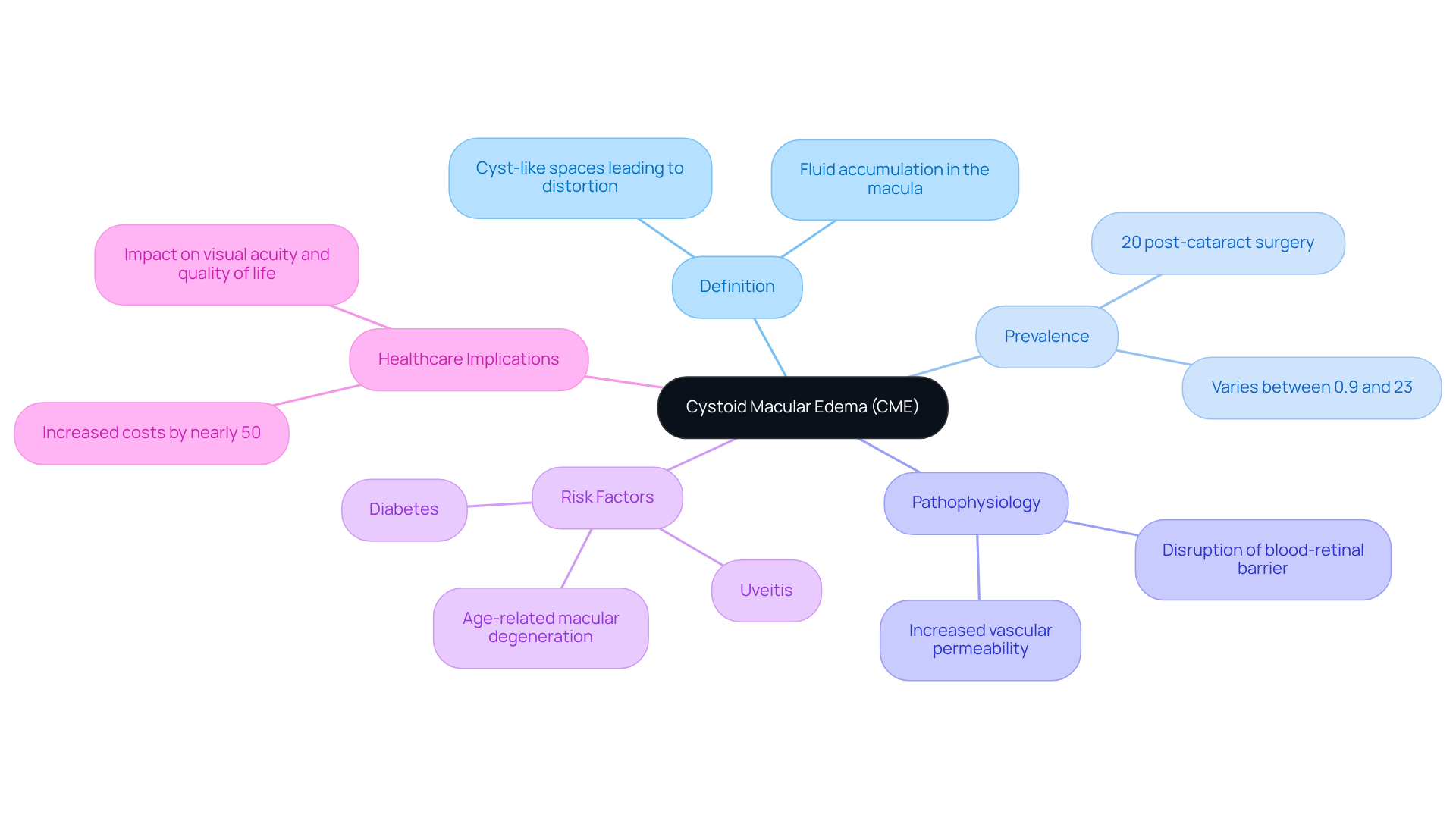
Cystoid macular edema (CME) understandably causes concern, as it involves fluid accumulation in the macula, which is the central part of the retina essential for sharp and detailed vision. This fluid buildup creates cyst-like spaces, leading to swelling and distortion of the macula, which can significantly impact visual acuity.
It’s important to know that cystoid macular edema often occurs as a complication of various ocular conditions or surgical procedures, particularly cataract surgery. In fact, approximately 20% of individuals may develop this condition after the operation. Recent studies reveal that the prevalence of CME following cataract surgery can vary widely, with rates reported between 0.9% and 23%, influenced by individual risk factors and diagnostic methods.
The pathophysiology of CME involves the disruption of the blood-retinal barrier, resulting in increased vascular permeability and fluid leakage into the retinal layers. Common risk factors for CME include diabetes, uveitis, and age-related macular degeneration.
Beyond affecting sight, CME can lead to increased healthcare costs, with a nearly 50% rise in expenses linked to cataract surgery in patients who experience this condition. Understanding cystoid macular edema is crucial for . Early intervention can significantly improve treatment outcomes and help restore visual function.
If you are experiencing blurred vision or other symptoms, we understand how concerning this can be. It is crucial to seek professional medical help immediately. We are here to help you through this process.
Identify Causes and Risk Factors of Cystoid Macular Edema
Cystoid macular edema can develop due to various causes, each adding to the complexity of the condition. We understand that navigating these factors can be overwhelming, so let’s explore some key contributors together:
- Post-surgical inflammation: CME is commonly observed following cataract surgery. This often occurs due to inflammatory responses that disrupt the blood-retinal barrier. Typically, postoperative CME arises within 3 months of surgery, peaking around 4-6 weeks after the procedure and impacting many individuals.
- Diabetes: If you have diabetes, it’s important to know that diabetic retinopathy is a notable risk factor for CME. Vascular changes in the retina can lead to fluid accumulation. Research indicates that individuals with diabetes have a relative risk of 2.87 for developing CME. This underscores the necessity for careful monitoring of cystoid macular edema in this group. As Sean McCafferty noted, “Topical nepafenac 0.3% significantly reduces the incidence of PCME compared to placebo when used after routine cataract surgery.”
- Uveitis: Inflammation of the uveal tract can compromise the integrity of the blood-retinal barrier, resulting in fluid leakage and subsequent CME. It’s common to feel concerned about cystoid macular edema, a condition that often requires careful management to prevent vision loss.
- Retinal vein occlusion: Blockages in retinal veins can elevate pressure within the eye, leading to fluid leakage and the development of CME. The risk is especially pronounced for individuals with pre-existing vascular conditions.
- Medications: Some medications, particularly prostaglandin analogs used in glaucoma treatment, have been associated with an increased risk of CME. Understanding these is essential for both patients and healthcare providers.
Recognizing these causes and risk factors is vital for effective management and prevention of cystoid macular edema (CME). The prevalence rates of CME can range from 0.9% to 23%, depending on the diagnostic method and the presence of risk factors. Furthermore, the development of CME can increase the costs associated with cataract surgery by an estimated 47%. By understanding the interplay between these elements, you can work closely with your healthcare providers to mitigate risks and enhance your overall eye health. Remember, we are here to help you through this process.

Recognize Symptoms of Cystoid Macular Edema
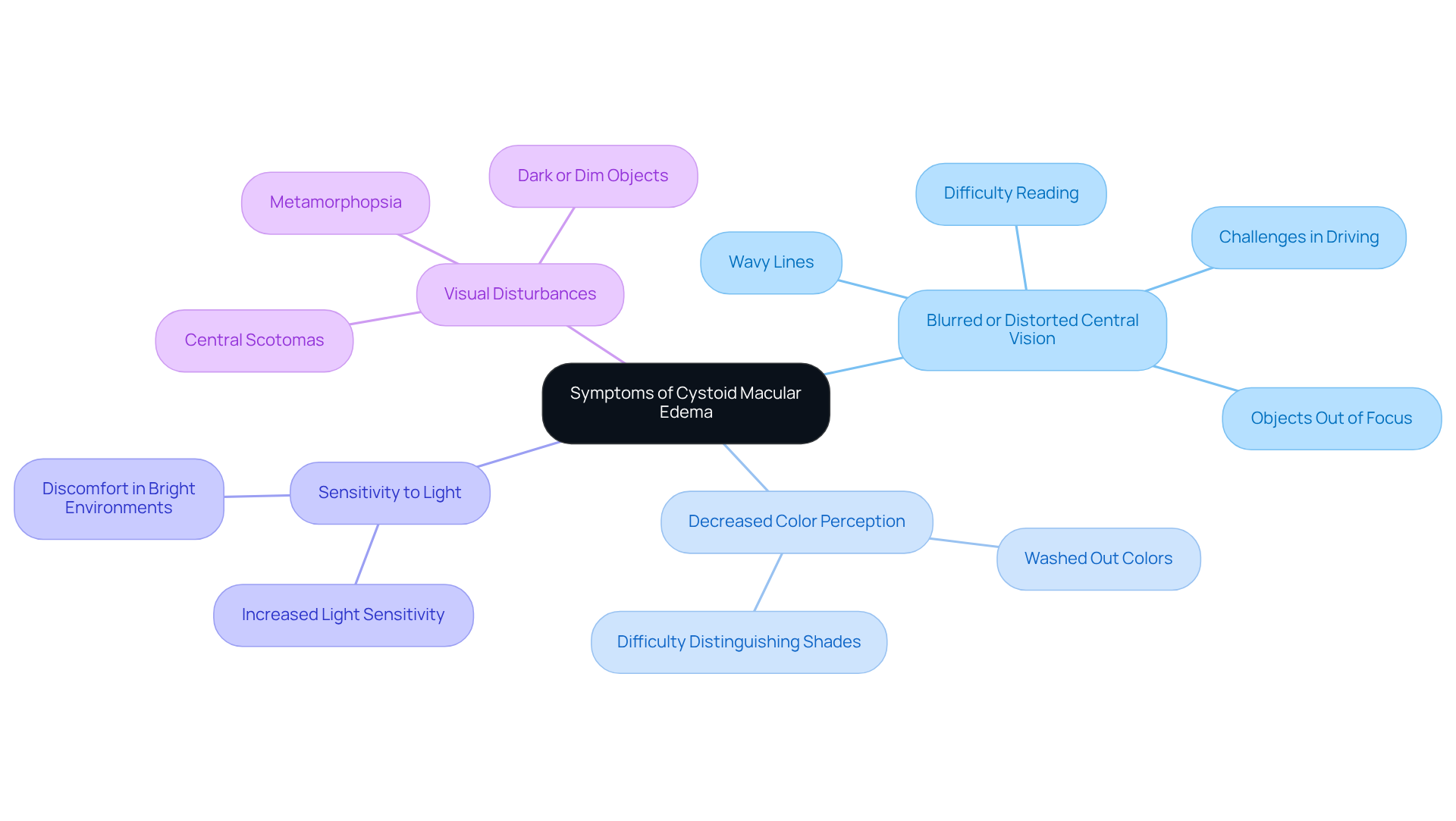
Cystoid macular edema (CME) can have a significant impact on your vision, and we recognize how troubling this can be. Here are some common symptoms you may experience:
- Blurred or distorted central vision: Many patients describe straight lines as wavy or objects appearing out of focus. This distortion can be disorienting and may impact daily activities like reading and driving.
- Decreased color perception: You might notice that colors seem washed out or less vibrant, which can change your visual experience and make it harder to distinguish between shades.
- Sensitivity to light: Increased sensitivity to bright environments is common, making it uncomfortable to be in well-lit areas.
- Visual disturbances: Some individuals may encounter central scotomas, which are blind spots in their central vision, or metamorphopsia, where objects appear distorted.
Recognizing these symptoms early is crucial, as timely intervention can lead to effective treatment and help maintain your sight. Research indicates that 1 to 3 percent of individuals undergoing cataract surgery may experience blurred vision due to cystoid macular edema, a common cause of reduced sight quality after the procedure. It’s reassuring to know that CME often resolves on its own within a few months. While peripheral vision typically remains unaffected, it’s essential to if you notice any changes in your vision. Additionally, managing underlying conditions like diabetes and high blood pressure can help lower the risk of developing cystoid macular edema (CME). We are here to help you through this process.
Explore Diagnostic Testing for Cystoid Macular Edema
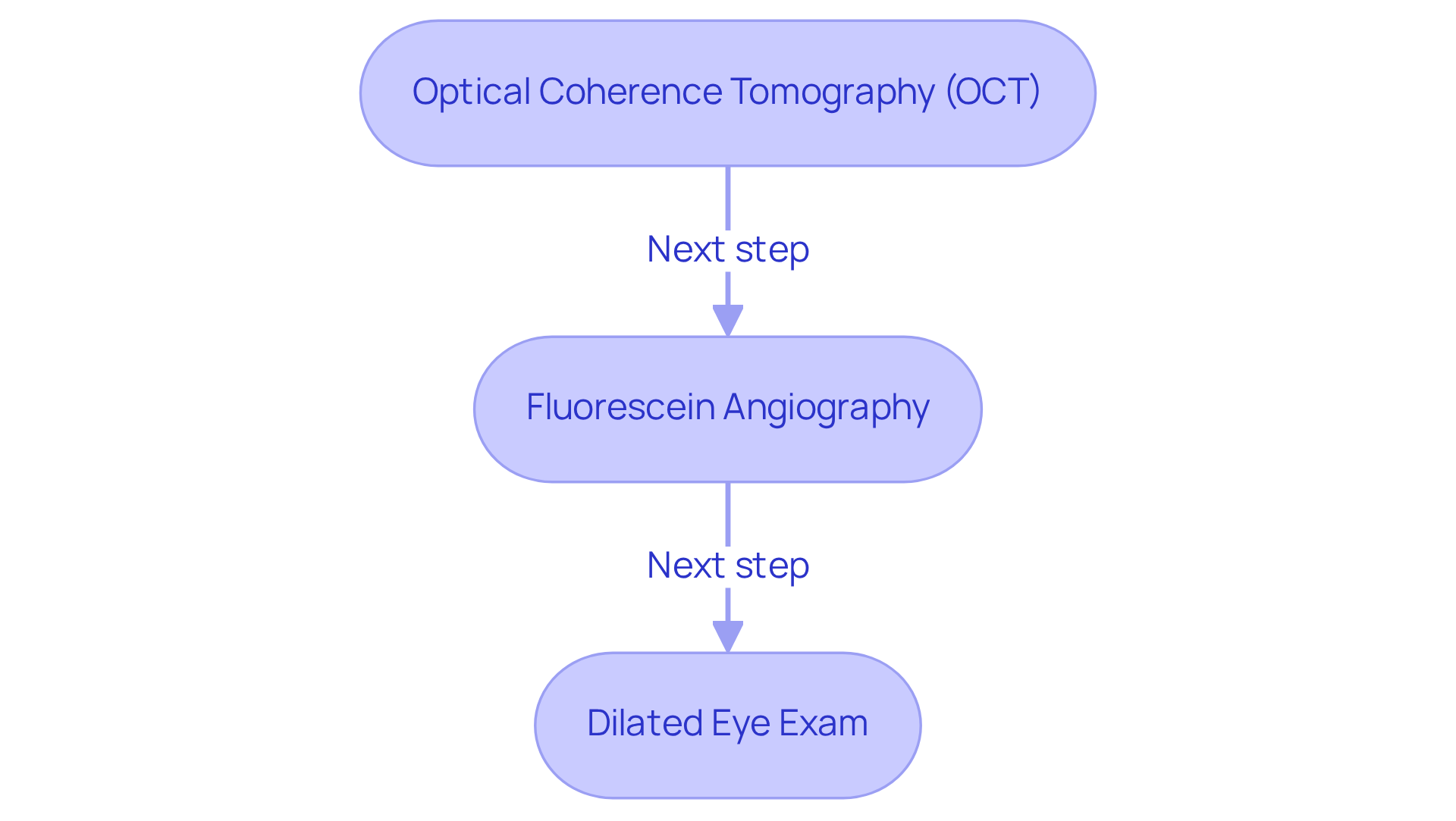
Diagnosing cystoid macular edema (CME) involves several critical tests that provide a comprehensive view of the condition, and we understand that this process can feel overwhelming:
- Optical Coherence Tomography (OCT): This advanced, non-invasive imaging technique offers detailed cross-sectional images of the retina, enabling precise assessment of macular thickness and fluid accumulation. OCT is particularly valuable for detecting subtle changes in the retina that may indicate CME, making it a cornerstone in the diagnostic process.
- Fluorescein Angiography: In this procedure, a fluorescent dye is injected into the bloodstream, allowing for the capture of photographs of the retina. This technique visualizes blood flow and identifies areas of leakage, which are crucial for diagnosing cystoid macular edema and evaluating its severity.
- Dilated Eye Exam: During this examination, an ophthalmologist uses specialized lenses to thoroughly inspect the retina for signs of CME and other retinal conditions. This hands-on evaluation complements the imaging techniques, providing a comprehensive view of your eye health.
These diagnostic tools are crucial for verifying the existence of cystoid macular edema and assessing its severity, which subsequently directs suitable options for your care. Notably, cystoid macular edema (CME) was diagnosed in 25,595 eyes, representing 0.8% of cataract surgeries, which underscores the importance of these diagnostic methods. The average onset of cystoid macular edema occurs approximately 6 weeks post-surgery, highlighting the critical window for diagnosis and intervention. Moreover, individuals diagnosed with cystoid macular edema (CME) had an average best-recorded visual acuity of 20/30 at postoperative month 12, emphasizing the necessity for early detection and intervention. We encourage after care, as they are crucial to prevent recurrence and ensure optimal outcomes. Remember, we are here to help you through this process.
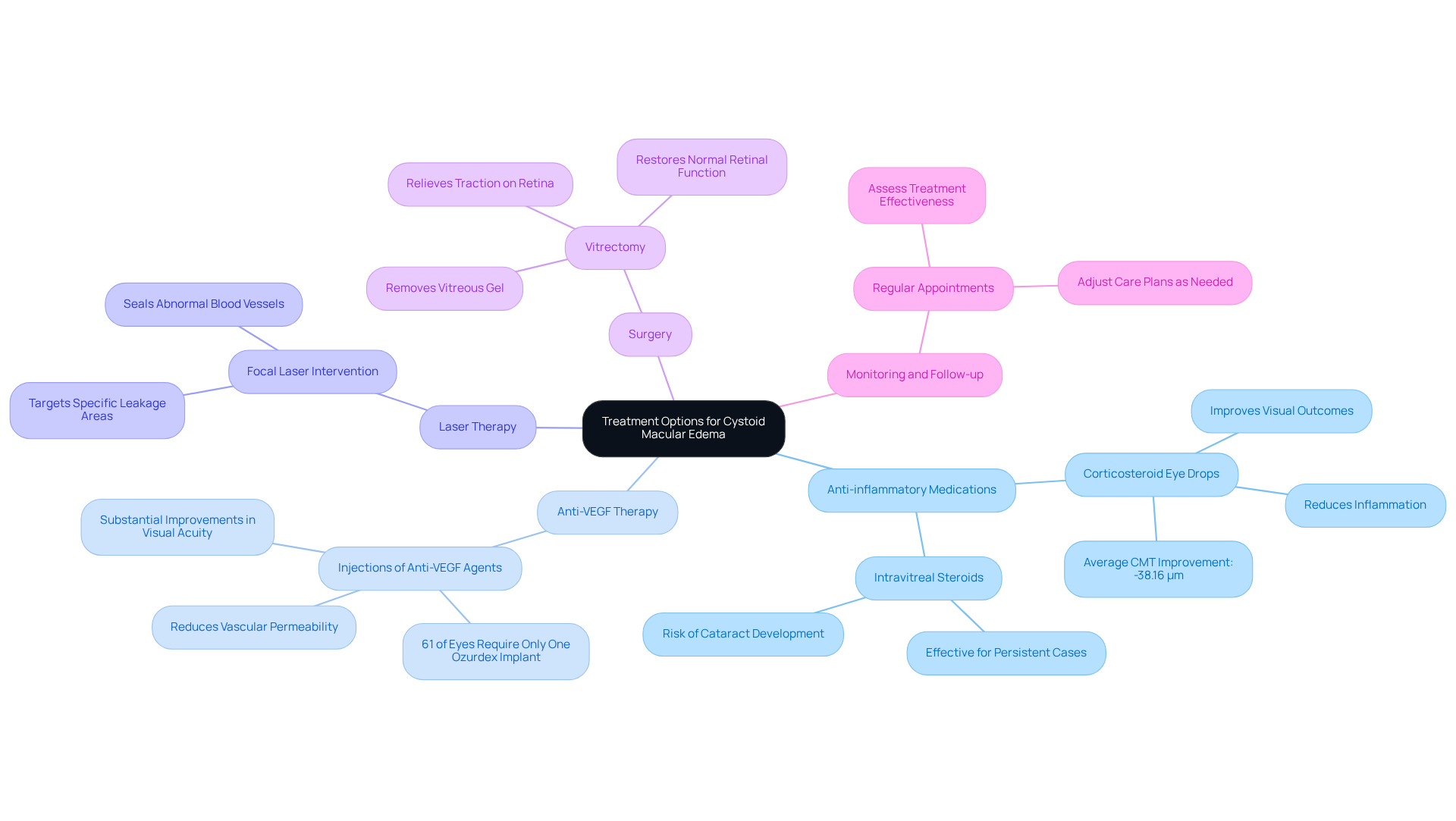
Review Treatment Options for Cystoid Macular Edema
When dealing with cystoid macular edema (CME), it’s natural to feel concerned about your eye health. Understanding the treatment options available can empower you to take charge of your well-being. The approaches to managing cystoid macular edema (CME) focus on reducing inflammation and fluid accumulation in the retina, and we are here to guide you through these choices.
- Anti-inflammatory medications are often the first line of defense. Corticosteroid eye drops or injections can significantly reduce inflammation and fluid buildup. Many patients have experienced improved visual outcomes, especially when inflammation is a primary concern. Research shows an average improvement in central macular thickness (CMT) of -38.16 μm after treatment, demonstrating their effectiveness.
- Another option is anti-VEGF therapy, which involves injections of anti-vascular endothelial growth factor agents. This treatment effectively reduces vascular permeability and fluid leakage. Studies indicate that patients receiving anti-VEGF therapy often see substantial improvements in visual acuity and central macular thickness. In fact, one study found that 61% of eyes required only a single Ozurdex implant for effective care.
- For those with localized fluid accumulation, laser therapy can be particularly beneficial. Focal laser intervention targets specific areas of leakage in the retina, helping to seal off abnormal blood vessels and reduce edema. This targeted approach can provide relief and improve your condition.
- In more severe cases where other methods may not work, surgery may be an option. Vitrectomy involves removing the vitreous gel to relieve traction on the retina, which can help restore normal retinal function. We understand that the thought of surgery can be daunting, but it can be a .
- Regular monitoring and follow-up appointments are essential to assess the effectiveness of your care and make any necessary adjustments. Staying informed about your eye health and actively engaging in your care plan is crucial.
Comprehending these treatment alternatives empowers you to make informed decisions and fosters collaboration with your healthcare providers. Remember, untreated cystoid macular edema can lead to irreversible vision loss, highlighting the importance of seeking timely treatment. We are here to help you through this process, ensuring you feel supported every step of the way.
Conclusion
Cystoid macular edema (CME) is a significant ocular condition that can be concerning, as it involves fluid accumulation in the macula, leading to distortion and compromised vision. We understand that learning about its causes, symptoms, diagnostic methods, and treatment options is essential for effective management and prevention of potential vision loss.
This article has explored various aspects of CME, including its association with:
- Cataract surgery
- Diabetes
- Uveitis
- Other risk factors that contribute to its development
Symptoms such as:
- Blurred vision
- Decreased color perception
- Sensitivity to light
are important to recognize early. It’s common to feel anxious about these symptoms, which is why early recognition and intervention are crucial.
Diagnostic techniques like Optical Coherence Tomography and fluorescein angiography play a vital role in confirming the presence of CME. Treatment options vary, ranging from anti-inflammatory medications to surgical interventions, depending on the severity of the condition. We want to reassure you that there are effective treatments available.
Ultimately, the significance of timely diagnosis and appropriate treatment cannot be overstated. If you experience any symptoms of CME, we encourage you to seek medical advice promptly. It’s important to explore your options and mitigate the risks of vision deterioration. By staying informed and proactive about your eye health, you can work collaboratively with healthcare professionals to ensure optimal outcomes and preserve your vision. Remember, we are here to help you through this process.
Frequently Asked Questions
What is cystoid macular edema (CME)?
Cystoid macular edema (CME) is a condition characterized by fluid accumulation in the macula, the central part of the retina, leading to swelling and distortion that can significantly impact visual acuity.
What are the common causes of cystoid macular edema?
Common causes of CME include post-surgical inflammation (especially after cataract surgery), diabetes, uveitis, retinal vein occlusion, and certain medications, particularly prostaglandin analogs used in glaucoma treatment.
How prevalent is cystoid macular edema after cataract surgery?
Approximately 20% of individuals may develop CME after cataract surgery, with prevalence rates reported between 0.9% and 23%, influenced by individual risk factors and diagnostic methods.
What are the risk factors associated with cystoid macular edema?
Risk factors for CME include diabetes (with a relative risk of 2.87), uveitis, age-related macular degeneration, and pre-existing vascular conditions.
How does cystoid macular edema affect healthcare costs?
The development of CME can increase healthcare costs by nearly 50% in patients undergoing cataract surgery.
What symptoms should prompt a visit to a healthcare professional regarding cystoid macular edema?
Symptoms such as blurred vision or other visual disturbances should prompt immediate medical attention, as early intervention can improve treatment outcomes.
What is the pathophysiology behind cystoid macular edema?
The pathophysiology of CME involves the disruption of the blood-retinal barrier, leading to increased vascular permeability and fluid leakage into the retinal layers.