Posted by: Northwest Eye in General on August 19, 2025
Overview
This article thoughtfully evaluates various medication options for Dry Eye Syndrome (DES) and how they can be tailored to meet individual needs. We understand that navigating treatment choices can be overwhelming, so we discuss the effectiveness, pros, and cons of options like artificial tears, cyclosporine, and intense pulsed light therapy.
It’s essential to recognize the importance of personalized treatment plans that consider your symptom severity, underlying causes, and lifestyle. By addressing these factors, we hope to empower you in your journey toward relief.
Introduction
Dry eye syndrome (DES) affects millions, often leading to discomfort and frustration in daily life. We understand how this condition can impact your well-being.
With a growing array of medications available, understanding the nuances of each option becomes essential for effective relief. Yet, it’s common to feel overwhelmed when navigating the maze of treatments to find the most suitable solution.
This article delves into the various medications for dry eye syndrome, comparing their effectiveness, benefits, and potential drawbacks. Our goal is to empower you in making informed choices for your eye health, reassuring you that we are here to help you through this process.
Understand Dry Eye Syndrome: Causes and Symptoms
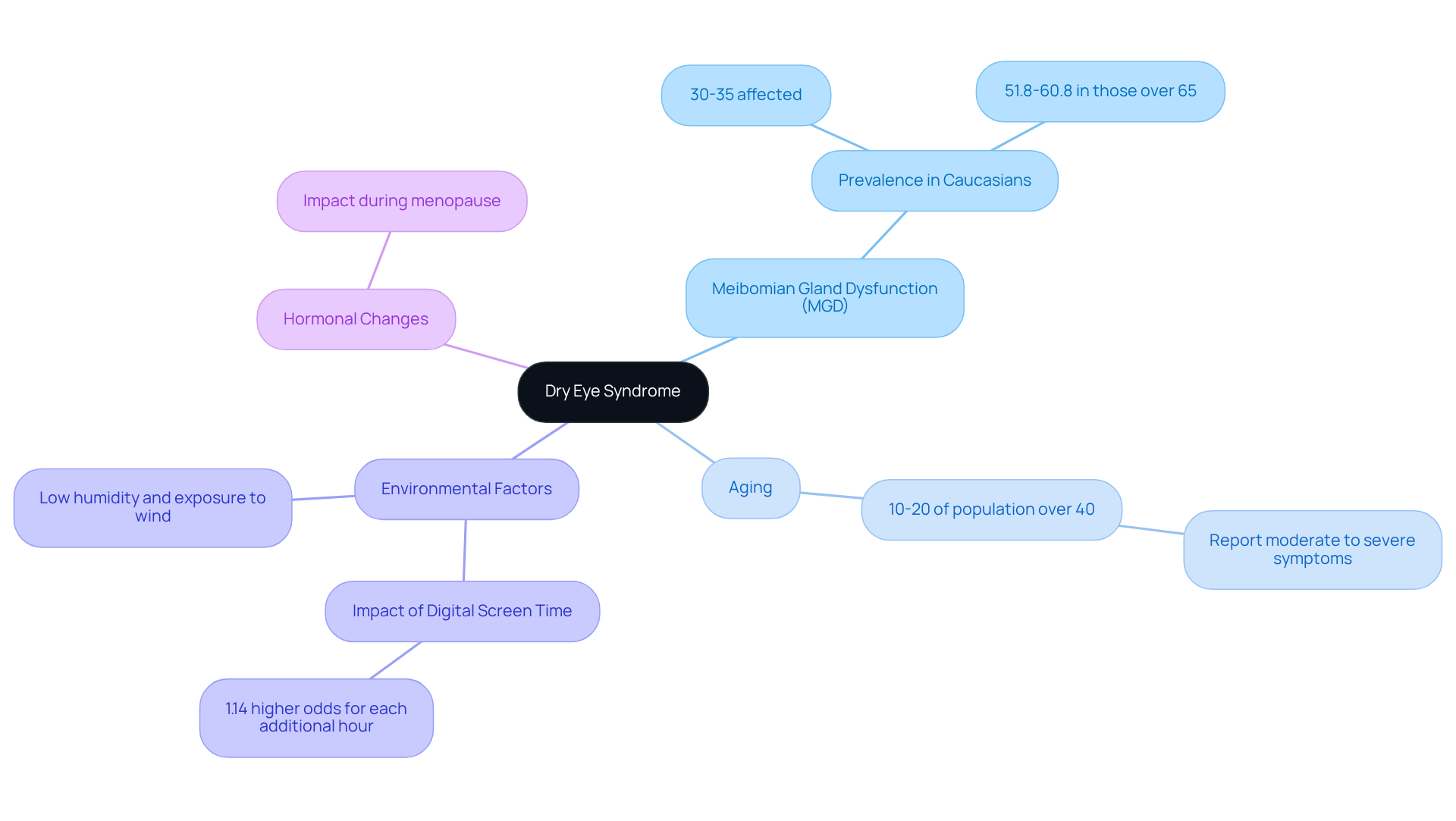
Dry eye syndrome (DES) is a common condition that many people face, characterized by insufficient fluid production or poor liquid quality. This can lead to inflammation and harm to the ocular surface, which can understandably be concerning. Let’s explore some key contributors to this condition:
- Meibomian Gland Dysfunction (MGD): This primary cause occurs when the oil-producing glands in the eyelids do not function effectively, leading to accelerated tear evaporation. It’s important to note that studies indicate MGD affects 30-35% of Caucasian individuals, with prevalence rates rising to 51.8-60.8% in those over 65 years.
- Aging: As we grow older, tear production tends to decrease, raising vulnerability to dry eye issues. Approximately 10-20% of the population over 40 years report moderate to severe signs of dry eye disease, and it’s common to feel frustrated by this change.
- Environmental Factors: Conditions such as low humidity, exposure to wind, smoke, and extended screen time can significantly worsen the effects of dry eyes. Research shows that every extra hour of digital screen use is associated with a 1.14 increased likelihood of experiencing dry eye issues, which many of us can relate to in today’s digital age.
- Hormonal Changes: Hormonal fluctuations, particularly during menopause, can impact tear production, contributing to the onset of dry eye syndrome. We understand that can be challenging.
Typical signs of DES include a gritty feeling, burning, redness, and varying vision. These indicators can greatly impact everyday tasks. In fact, research shows that 67% of individuals with dry eye disease have had to limit their daily activities because of their condition. Understanding these causes and symptoms is crucial for evaluating the effectiveness of various dry eye syndrome medication options available for treating dry eye syndrome. We are here to help you navigate these challenges, especially in light of the growing prevalence of MGD and its implications for patient care.
Explore Available Medications for Dry Eye Treatment
If you’re experiencing dry eye syndrome, it’s important to know that dry eye syndrome medication can help you find relief, each with its own unique way of working. We understand how uncomfortable this condition can be, and we’re here to support you in .
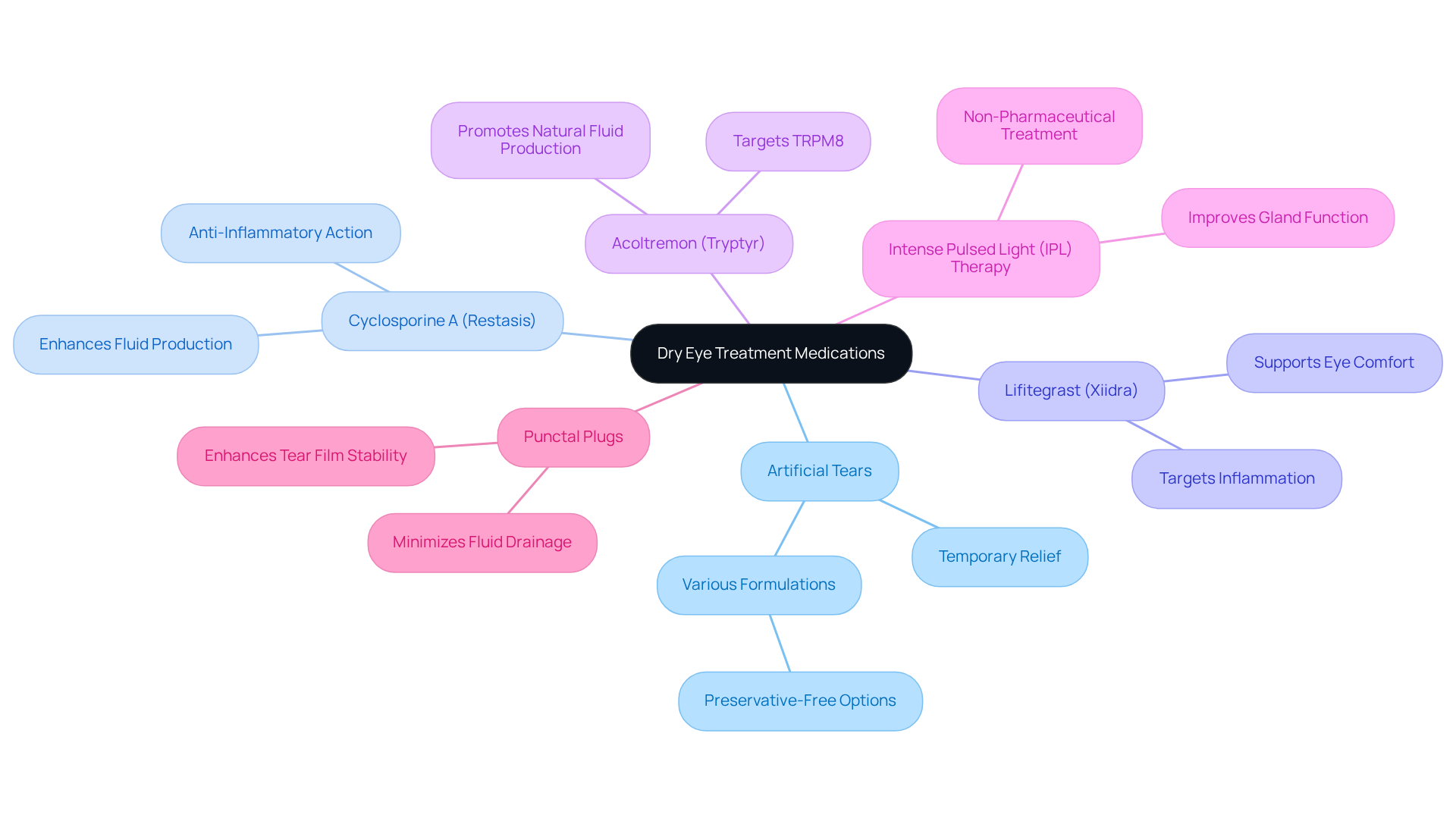
- Artificial Tears: These over-the-counter lubricating eye drops provide temporary relief by supplementing your natural tears. They come in various viscosities and formulations, including preservative-free options that are gentle on sensitive eyes.
- Cyclosporine A (Restasis): This dry eye syndrome medication works as an anti-inflammatory to enhance fluid production by reducing inflammation on the ocular surface, helping to soothe your eyes.
- Lifitegrast (Xiidra): Another anti-inflammatory option, Lifitegrast targets the underlying inflammation associated with dry eye disease, making it a beneficial dry eye syndrome medication that offers you additional support.
- Acoltremon (Tryptyr): A newer eye drop that targets TRPM8, promoting natural fluid production. Recent studies show it holds promise for those seeking relief.
- Intense Pulsed Light (IPL) Therapy): This non-pharmaceutical treatment focuses on meibomian gland dysfunction (MGD) by reducing inflammation and improving gland function, which can be a game-changer for your comfort.
- Punctal Plugs: These small devices are placed in the duct openings to minimize fluid drainage, helping to enhance the stability of your tear film.
Each of these options has its own indications, benefits, and potential side effects. It’s crucial to evaluate them in the context of your individual needs. Remember, you’re not alone in this journey, and we are here to help you find the best solution for your eyes.
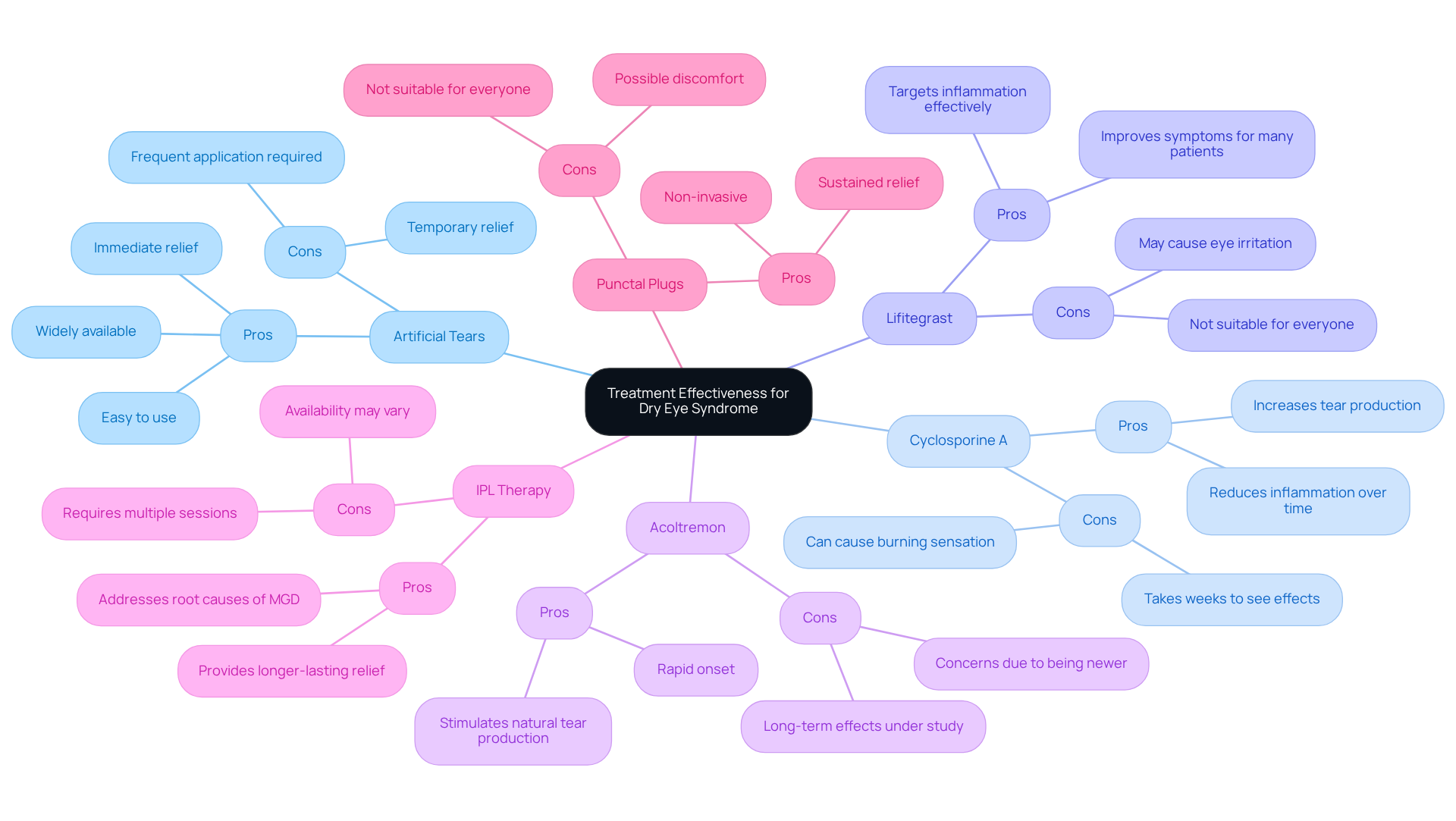
Compare Treatment Effectiveness: Pros and Cons of Each Medication
-
Medication: Artificial Tears
- Pros: Widely available, easy to use, and provides immediate relief for many.
- Cons: While they offer temporary relief, they may require frequent application.
-
Medication: Cyclosporine A
- Pros: This option can increase tear production and reduce inflammation over time.
- Cons: However, it may take weeks to see effects and can cause a burning sensation for some.
-
Medication: Lifitegrast
- Pros: It effectively targets inflammation and improves symptoms for many patients.
- Cons: Some may experience eye irritation, and it may not be suitable for everyone.
-
Medication: Acoltremon
- Pros: This newer treatment stimulates natural tear production with a rapid onset.
- Cons: Being newer, its long-term effects are still under study, which may raise concerns.
-
Medication: IPL Therapy
- Pros: This therapy addresses the root causes of meibomian gland dysfunction (MGD) and often provides longer-lasting relief.
- Cons: It does require multiple sessions, and availability may vary, which can be a hurdle.
-
Medication: Punctal Plugs
- Pros: They offer sustained relief and are non-invasive, making them a comforting choice.
- Cons: Some patients might experience discomfort, and they are not suitable for everyone.
This comparison highlights the diverse treatment options available for dry eye syndrome. We understand that navigating these choices can be overwhelming, but that include dry eye syndrome medication tailored to your unique needs and responses are essential. We are here to help you through this process.
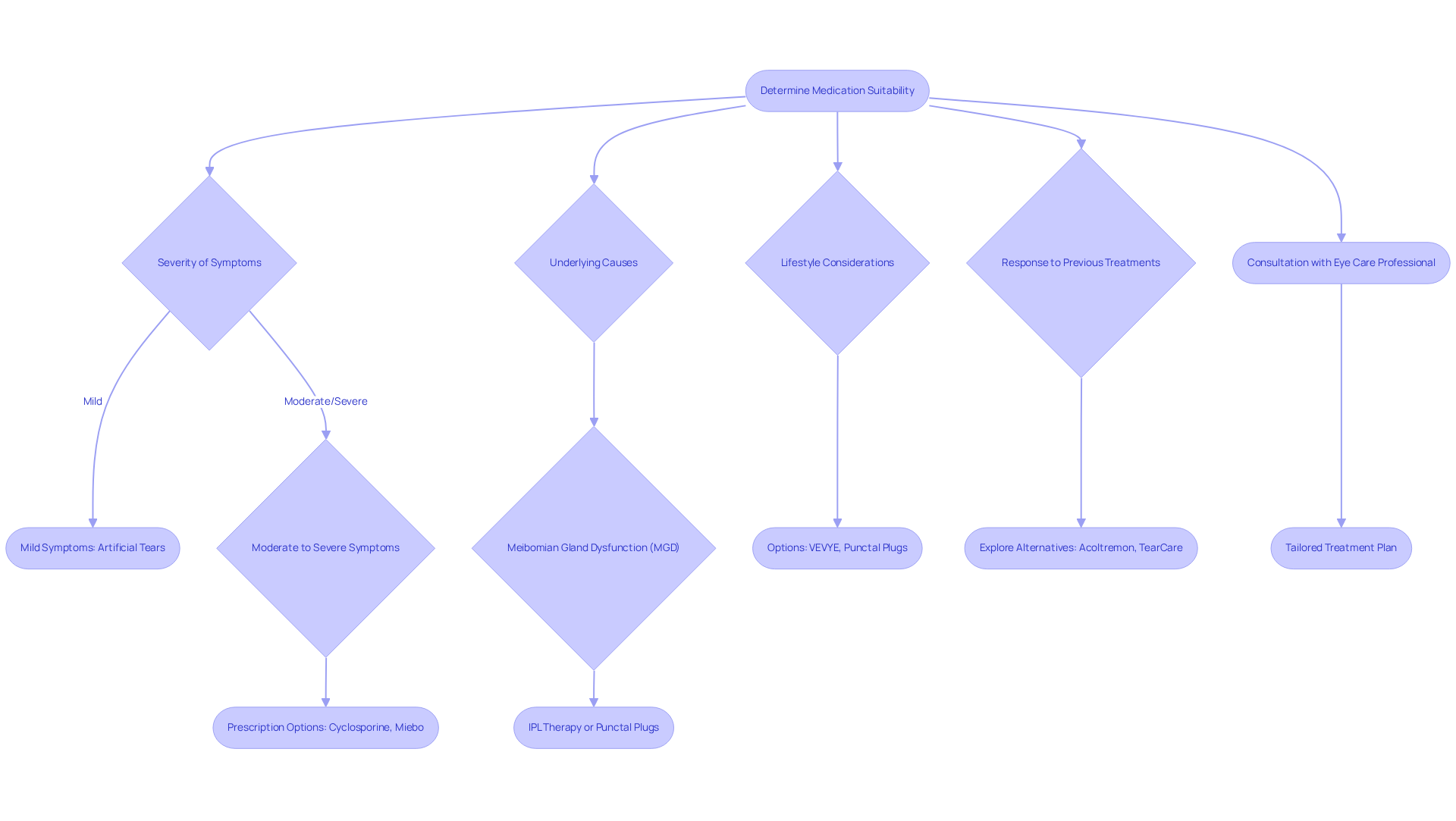
Determine Suitability: Which Medication Fits Your Needs?
Selecting the appropriate dry eye syndrome medication involves careful consideration of various factors, and we understand that navigating this can feel overwhelming.
- Severity of Symptoms: If you have mild symptoms, artificial tears may provide relief. However, for those experiencing moderate to severe symptoms, prescription options like cyclosporine or newer treatments such as Miebo— the first FDA-approved dry eye syndrome medication for dry eye associated with Meibomian gland dysfunction— may be necessary. These treatments specifically target excessive tear evaporation, offering hope for improved comfort.
- Underlying Causes: For individuals with meibomian gland dysfunction (MGD), effective treatments like intense pulsed light (IPL) therapy or punctal plugs can make a significant difference. IPL therapy, which received FDA approval in 2021, helps reduce inflammation and enhances fluid quality. A case study on TearCare highlights its effectiveness for MGD, noting that patients typically need to repeat the procedure every three months to maintain optimal results.
- Lifestyle Considerations: We recognize that busy schedules can make consistent treatment challenging. Options like VEVYE, a preservative-free cyclosporine drop, or punctal plugs offer longer-lasting relief without the need for multiple daily applications, allowing you to focus on your daily life while managing your symptoms.
- Response to Previous Treatments: If your previous medication has not provided the relief you hoped for, exploring alternatives may be beneficial. Treatments like Acoltremon, which stimulates tear production, or the TearCare procedure for MGD could be advantageous. As Dr. Nishika Reddy emphasizes, a combination of ongoing therapies often proves effective in managing these issues.
- Consultation with an Eye Care Professional: A comprehensive evaluation by an ophthalmologist is crucial. They can assess the severity of your symptoms and recommend tailored treatment plans that align with your individual needs and preferences.
Ultimately, a collaborative approach between you and your healthcare provider is essential for identifying the most effective and convenient dry eye syndrome medication for managing the condition. With dry eye disease affecting almost 20 million people in the U.S., seeking is vital, and we are here to help you through this process.
Conclusion
Understanding dry eye syndrome and its various treatment options is essential for anyone affected by this common condition. We recognize that dealing with dry eye can be uncomfortable and frustrating. This article highlights the complexity of dry eye syndrome, emphasizing the importance of evaluating the underlying causes and the suitability of different medications. By exploring the array of available treatments, from artificial tears to innovative therapies like intense pulsed light, individuals can make informed decisions that cater to their specific needs and circumstances.
The key points discussed include the multifaceted causes of dry eye syndrome, such as:
- Meibomian gland dysfunction
- Environmental factors
- Hormonal changes
We understand that each person’s experience is unique, and it’s common to feel overwhelmed by the options. Each medication option, including their pros and cons, has been examined to provide a comprehensive overview of what may work best for different severity levels and underlying issues. Furthermore, the necessity of consulting with a healthcare professional to tailor a treatment plan is underscored, ensuring that each person’s unique situation is taken into account.
Ultimately, addressing dry eye syndrome requires a proactive approach in selecting the right medication and treatment strategy. We are here to help you through this process. As the landscape of dry eye treatments continues to evolve, staying informed about the latest options and understanding how to evaluate them is crucial. Those experiencing dry eye symptoms are encouraged to seek personalized solutions that not only alleviate discomfort but also enhance their quality of life.
Frequently Asked Questions
What is dry eye syndrome (DES)?
Dry eye syndrome is a common condition characterized by insufficient fluid production or poor liquid quality in the eyes, leading to inflammation and potential harm to the ocular surface.
What are the primary causes of dry eye syndrome?
The primary causes of dry eye syndrome include Meibomian Gland Dysfunction (MGD), aging, environmental factors, and hormonal changes.
What is Meibomian Gland Dysfunction (MGD)?
MGD occurs when the oil-producing glands in the eyelids do not function effectively, resulting in accelerated tear evaporation. It affects 30-35% of Caucasian individuals, with higher prevalence rates in those over 65 years.
How does aging affect dry eye syndrome?
As individuals age, tear production typically decreases, increasing the risk of dry eye issues. Approximately 10-20% of the population over 40 years report moderate to severe signs of dry eye disease.
What environmental factors can worsen dry eye symptoms?
Low humidity, exposure to wind, smoke, and extended screen time can significantly exacerbate dry eye symptoms. Research indicates that each additional hour of digital screen use is associated with a higher likelihood of experiencing dry eye issues.
How do hormonal changes contribute to dry eye syndrome?
Hormonal fluctuations, particularly during menopause, can affect tear production, leading to the onset of dry eye syndrome.
What are the typical symptoms of dry eye syndrome?
Typical symptoms include a gritty feeling, burning sensation, redness, and varying vision. These symptoms can significantly impact daily activities.
How does dry eye syndrome affect daily life?
Research shows that 67% of individuals with dry eye disease have had to limit their daily activities due to their condition, highlighting its impact on everyday tasks.
Why is it important to understand the causes and symptoms of dry eye syndrome?
Understanding the causes and symptoms of dry eye syndrome is crucial for evaluating the effectiveness of various medication options available for treating the condition.