Posted by: Northwest Eye in General on September 3, 2025
Overview
Keratoplasty is a surgical procedure that involves the transplantation of corneal tissue. It is performed to restore vision and enhance corneal integrity. There are various techniques available, depending on the specific eye condition. We understand that undergoing surgery can be a daunting experience, and it’s common to have many questions.
In this article, we will outline the steps of the procedure, what to expect during recovery, potential complications, and the generally favorable outcomes. Understanding these aspects can help you prepare for your surgical journey. Remember, you are not alone in this process; we are here to help you through it.
As you read, you may find comfort in knowing that many patients have successfully navigated this experience. Their stories often highlight the importance of preparation and support. We encourage you to reach out with any questions or concerns you may have about keratoplasty.
Your journey towards improved vision and eye health is important, and we are committed to providing you with the information and support you need. Together, we can work towards a brighter future for your eyesight.
Introduction
Keratoplasty is a vital surgical intervention that can restore vision, offering hope to those facing various ocular conditions. This article explores the intricacies of keratoplasty, including its types, the procedural steps involved, and the recovery journey that follows.
We understand that considering surgery can be daunting, and you may have important questions:
- What are the risks?
- How can you ensure the best possible outcomes?
It’s common to feel this way, and understanding these factors is crucial for anyone contemplating this transformative procedure. We are here to help you through this process.
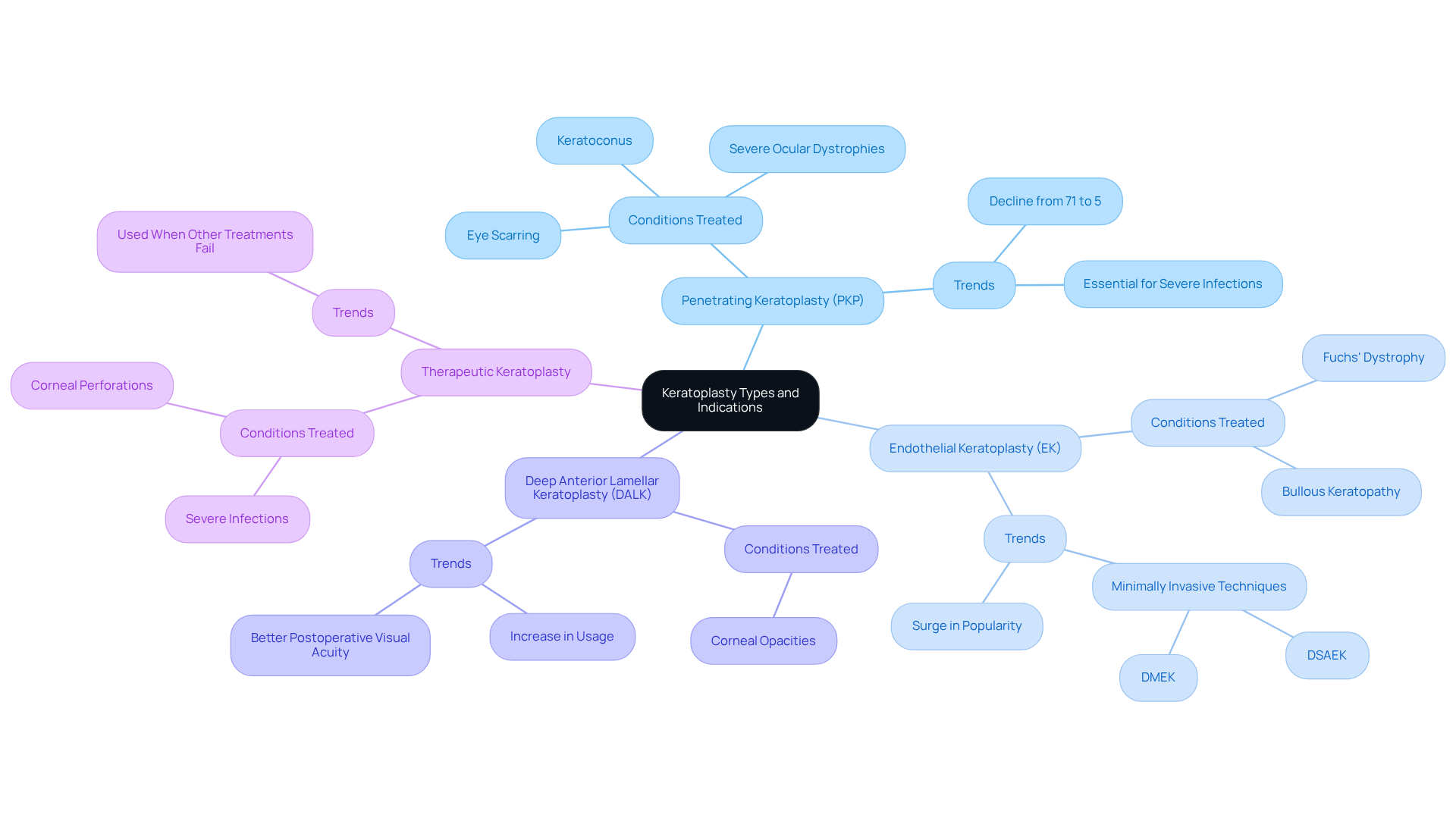
Define Keratoplasty: Types and Indications
The surgical procedure known as involves the transplantation of eye tissue to restore vision or enhance the integrity of the cornea. We understand that considering such a procedure can be daunting, and we are here to support you through this process. The types of keratoplasty include:
- Keratoplasty, specifically penetrating keratoplasty (PKP), involves a full-thickness transplant that replaces the entire eye surface with donor material. It is indicated for conditions such as eye scarring, keratoconus, and severe ocular dystrophies. Recent data indicates that keratoplasty remains essential for managing severe infections and perforations, although its overall proportion has declined significantly, from 71% to 5%. Knowing this can help reassure you that there are options available.
- Keratoplasty, specifically Endothelial Keratoplasty (EK), is a technique that replaces only the innermost layer of the cornea (the endothelium) and is typically used for conditions like Fuchs’ dystrophy and bullous keratopathy. The popularity of EK has surged, with techniques like Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemet membrane endothelial keratoplasty (DMEK) becoming favored choices because of their minimally invasive nature and faster recovery times. It’s common to feel hopeful about these advancements.
- Deep Anterior Lamellar Keratoplasty (DALK) is a technique that substitutes the front layers of the eye’s surface while preserving your own endothelium, making it suitable for individuals with corneal opacities but healthy endothelial cells. DALK has seen a notable increase in usage, reflecting a shift towards less invasive techniques that offer better postoperative visual acuity and faster rehabilitation. This can be an encouraging option for many patients.
- Keratoplasty is a therapeutic procedure performed to treat corneal perforations or severe infections, aiming to restore the structural integrity of the eye. It is often necessary in cases where other treatments have failed. We recognize the importance of addressing these serious conditions.
The selection of corneal surgery type is influenced by the particular state of your cornea and the intended surgical results. Current trends suggest a notable increase in lamellar procedures, especially DALK and EK, as they offer benefits like fewer complications and enhanced recovery durations. As of now, the occurrence of conditions addressed by corneal transplant continues to change, with bullous keratopathy and Fuchs endothelial dystrophy being among the primary reasons for these interventions. Remember, you are not alone in this journey, and we are here to help you every step of the way.
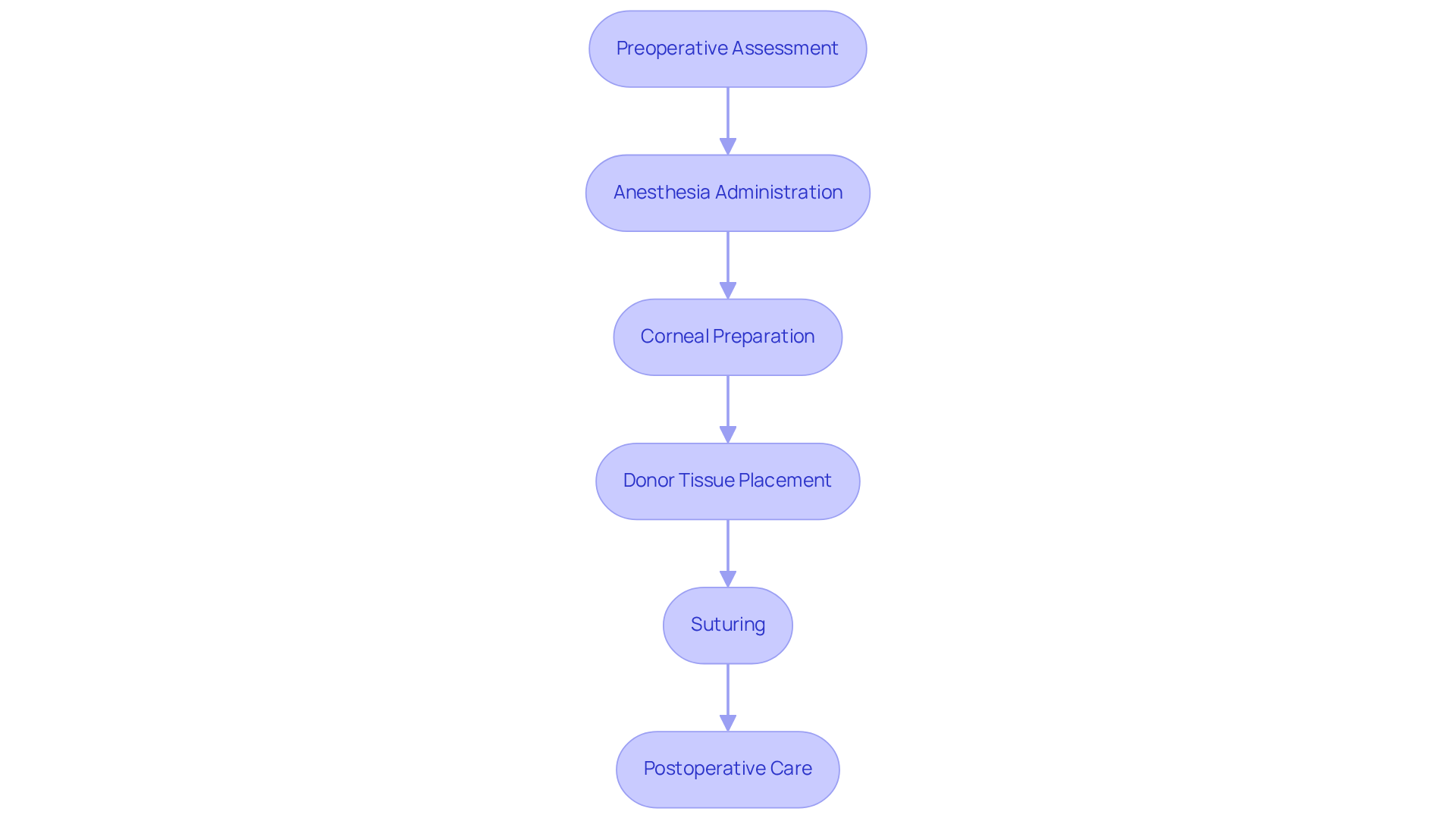
Explain the Keratoplasty Procedure: Step-by-Step Overview
The keratoplasty procedure typically unfolds through several key steps that we want you to feel comfortable with:
- Preoperative Assessment: We begin with a thorough eye examination, including imaging tests to assess corneal health. This step is essential, especially for individuals with conditions like keratoconus, as keratoplasty may be needed when the cornea has an abnormal curvature affecting vision.
- Anesthesia Administration: To ensure your comfort and pain relief during surgery, either local or general anesthesia will be provided based on your specific needs. Anesthesia is crucial in enhancing your surgical experience, allowing you to undergo the procedure without discomfort. As Dr. John H. Collins noted, “Anesthesia is the key to the modern practice of surgery.”
- Corneal Preparation: The surgeon will prepare your cornea by excising the damaged or diseased tissue. This is done using a trephine or microkeratome, depending on whether keratoplasty is performed as a penetrating keratoplasty (PKP) or an endothelial keratoplasty (EK). For those with keratoconus, specially fitted contact lenses may be recommended before surgery to help address corneal distortion.
- Donor Tissue Placement: The donor cornea is carefully positioned onto your eye. In PKP, the entire cornea is replaced, while in EK, only the endothelial layer is transplanted. These advancements in surgical techniques, particularly keratoplasty, aim to improve recovery and outcomes. The 5-year graft survival rate for DMEK techniques is reported to be between 90-95%, with rejection rates ranging from 0.7% to 5%. This information is particularly important for individuals with keratoconus, as can help prevent lasting vision impairment.
- Suturing: Fine sutures will secure the donor tissue in place, which may remain for several months to facilitate proper healing and integration of the graft.
- Postoperative Care: After the procedure, you will be closely monitored for any immediate complications. We will provide detailed postoperative care instructions, including the use of prescribed eye drops and scheduling follow-up appointments to ensure optimal recovery. It’s common to feel a mix of anxiety and hope before surgery, and understanding these steps can help ease your worries and prepare you for the experience. For those with keratoconus, grasping the potential outcomes of keratoplasty and the importance of follow-up care is vital for maintaining eye health.
By familiarizing yourself with these steps, you can feel more ready and informed about what to expect during your eye surgery. We are here to help you through this process.
Outline Recovery After Keratoplasty: Care and Expectations
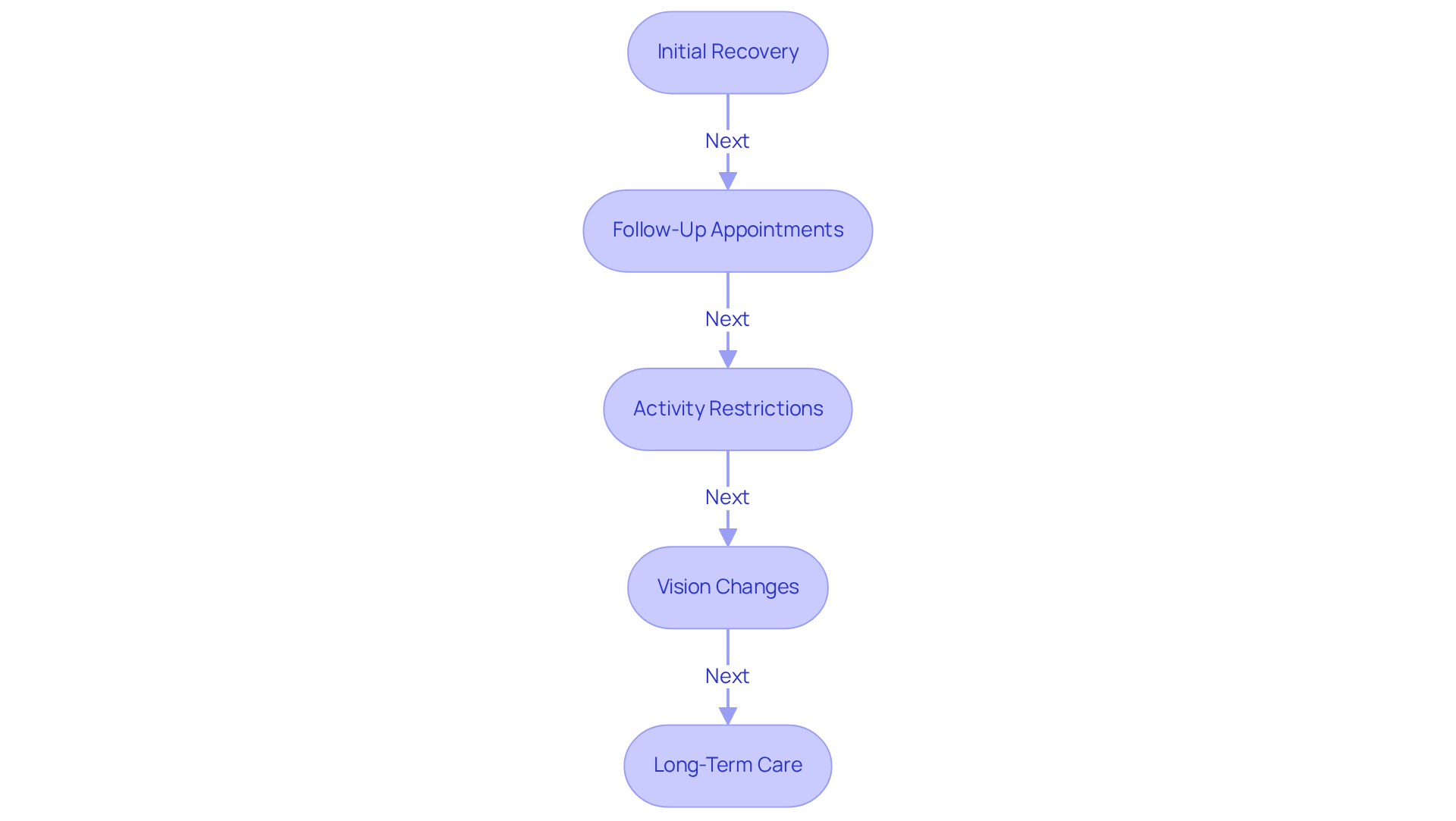
Recovery after keratoplasty can vary based on the specific procedure performed, but generally follows these key stages:
- Initial Recovery: We understand that shortly after surgery, you may experience discomfort, light sensitivity, and blurred vision. These symptoms can arise from the surgical procedure itself or underlying conditions such as uncorrected refractive errors, cataracts, or diabetic retinopathy. It’s important to know that these symptoms are typically managed with prescribed pain relief and anti-inflammatory medications, and in some cases, keratoplasty may be considered to ensure a more comfortable recovery.
- Follow-Up Appointments: Regular follow-up visits are essential for monitoring your healing after keratoplasty and for identifying any complications early. The first appointment usually occurs within 24 to 48 hours post-surgery, allowing your ophthalmologist to assess the initial healing process.
- Activity Restrictions: We want to remind you that to prevent complications, it’s advised to avoid strenuous activities, swimming, and rubbing your eyes for several weeks. These precautions are crucial for protecting the delicate surgical site during the early stages of recovery following keratoplasty.
- Vision Changes: It’s common to feel concerned about fluctuating vision during the recovery period. You should expect following keratoplasty, which can take weeks to months, depending on the type of eye surgery conducted. Understanding this variability helps set realistic expectations for your visual outcomes. Please be aware that blurred vision can indicate other issues, such as cataracts or diabetic retinopathy, which may require further evaluation.
- Long-Term Care: Adherence to your prescribed eye drop regimens is vital for preventing infection and managing inflammation following keratoplasty. You may need to use these medications for several months, and consistent follow-up care is essential to ensure a successful recovery and optimal long-term results. Remember, we are here to help you through this process.
Discuss Complications and Expected Outcomes of Keratoplasty
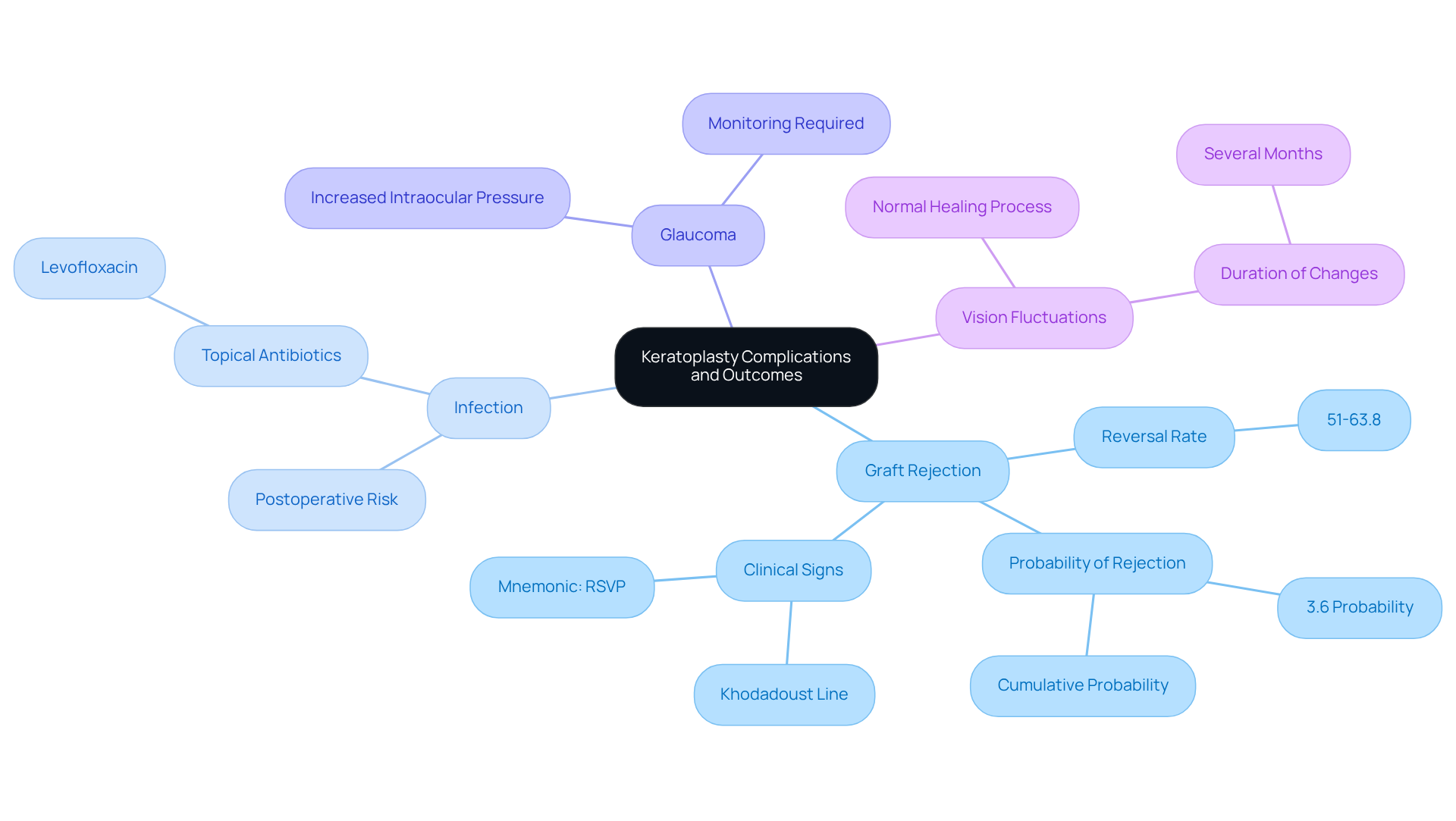
While the success rate of keratoplasty is high, we recognize the importance of being aware of . These may include:
- Graft Rejection: It’s natural to worry about the body rejecting donor tissue, which can lead to inflammation and potential loss of vision. Early detection and treatment are crucial, as the cumulative probability of definite graft rejection is approximately 3.6%. The reversal rate of eye tissue endothelial graft rejection varies from 51% to 63.8%. We encourage you to recognize clinical signs of graft rejection, such as corneal edema, keratic precipitates, and the Khodadoust line. A helpful mnemonic to remember is ‘RSVP’ (Redness, Sensitivity to Light, Vision, and Pain).
- Infection: Postoperative infections can occur, and we want you to know that prompt medical attention is vital to prevent serious complications. The application of topical antibiotics, like levofloxacin, is commonly used in the postoperative regimen to help mitigate this risk.
- Glaucoma: It’s common to experience increased intraocular pressure after surgery, which requires monitoring and management to prevent long-term damage.
- Vision Fluctuations: You may notice changes in your vision as your eye heals, which can take several months. This is a normal part of the recovery process, and discussing it with your healthcare provider can help ease any concerns you may have.
- Long-Term Outcomes: Many individuals observe considerable enhancements in vision after keratoplasty. Graft survival rates can differ based on the type of corneal surgery performed. For instance, penetrating keratoplasty (PKP) has a graft survival rate of approximately 90% at five years, while the Descemet’s Stripping Endothelial procedure (DSEK) has a rejection rate of about 10%, and the Descemet Membrane Endothelial technique (DMEK) has a rejection rate of approximately 1.9%. Understanding these aspects of keratoplasty is crucial for you, as it enables informed decisions and adequate preparation for your surgical journey. Remember, we are here to help you through this process.
Conclusion
Keratoplasty is a vital surgical procedure aimed at restoring vision and enhancing the cornea’s integrity through the transplantation of donor tissue. We understand that considering this intervention can bring about many emotions and questions. Therefore, it’s essential to familiarize yourself with the various types, including:
- Penetrating keratoplasty
- Endothelial keratoplasty
- Deep anterior lamellar keratoplasty
Each type serves specific conditions and offers unique benefits, highlighting the importance of personalized treatment options based on your individual corneal health.
Throughout this article, we’ve explored key aspects of the keratoplasty process, including the detailed steps from preoperative assessments to postoperative care. It’s common to feel uncertain about recovery expectations, potential complications, and long-term outcomes. We emphasize the importance of follow-up appointments and adherence to prescribed regimens. With a high success rate and advancements in surgical techniques, many patients can anticipate significant improvements in their vision.
Ultimately, the journey through keratoplasty is not just about the surgery itself but also about understanding the comprehensive care that follows. We encourage you to engage actively with your healthcare providers, stay informed about your recovery, and recognize the signs of potential complications. Embracing this knowledge empowers you to navigate your path toward improved vision and eye health effectively. Remember, we are here to help you through this process.
Frequently Asked Questions
What is keratoplasty?
Keratoplasty is a surgical procedure that involves the transplantation of eye tissue to restore vision or enhance the integrity of the cornea.
What are the main types of keratoplasty?
The main types of keratoplasty include Penetrating Keratoplasty (PKP), Endothelial Keratoplasty (EK), and Deep Anterior Lamellar Keratoplasty (DALK).
What conditions are treated with Penetrating Keratoplasty (PKP)?
PKP is indicated for conditions such as eye scarring, keratoconus, and severe ocular dystrophies.
How has the role of keratoplasty in managing severe infections changed?
The overall proportion of keratoplasty for managing severe infections and perforations has significantly declined, from 71% to 5%.
What is Endothelial Keratoplasty (EK) and when is it used?
EK is a technique that replaces only the innermost layer of the cornea (the endothelium) and is typically used for conditions like Fuchs’ dystrophy and bullous keratopathy.
What are the advantages of Endothelial Keratoplasty techniques like DSAEK and DMEK?
DSAEK and DMEK are favored for their minimally invasive nature and faster recovery times.
What is Deep Anterior Lamellar Keratoplasty (DALK)?
DALK is a technique that substitutes the front layers of the eye’s surface while preserving the patient’s own endothelium, suitable for individuals with corneal opacities but healthy endothelial cells.
Why is keratoplasty performed as a therapeutic procedure?
Keratoplasty is performed to treat corneal perforations or severe infections, aiming to restore the structural integrity of the eye when other treatments have failed.
What factors influence the selection of the type of keratoplasty?
The selection is influenced by the specific condition of the cornea and the intended surgical results.
What current trends are observed in corneal surgery?
There is a notable increase in lamellar procedures, especially DALK and EK, due to their benefits of fewer complications and enhanced recovery durations.