Posted by: Northwest Eye in General on October 8, 2025
Overview
Pachymetry is a vital diagnostic procedure that measures corneal thickness, and it plays a significant role in cataract care. We understand that you may have concerns about your eye health, and knowing your corneal thickness can help assess the risk of complications and guide treatment decisions.
Understanding pachymetry results allows you to engage in informed discussions about your eye health and treatment options. It’s common to feel uncertain, but rest assured that variations in corneal thickness can significantly influence surgical strategies and outcomes.
We are here to help you through this process.
Introduction
Pachymetry is a critical yet often overlooked diagnostic tool in eye care. It measures the thickness of the cornea, which is essential for ensuring successful cataract surgery and recovery. We understand that navigating eye health can be overwhelming, but by grasping the implications of these measurements, you can gain valuable insights into your eye health. This knowledge empowers you to make informed decisions regarding your treatment options.
It’s common to feel uncertain about how these details impact your care. However, the nuances of pachymetry can significantly transform not only surgical outcomes but also the overall management of ocular conditions. We are here to help you through this process, providing the support you need every step of the way.
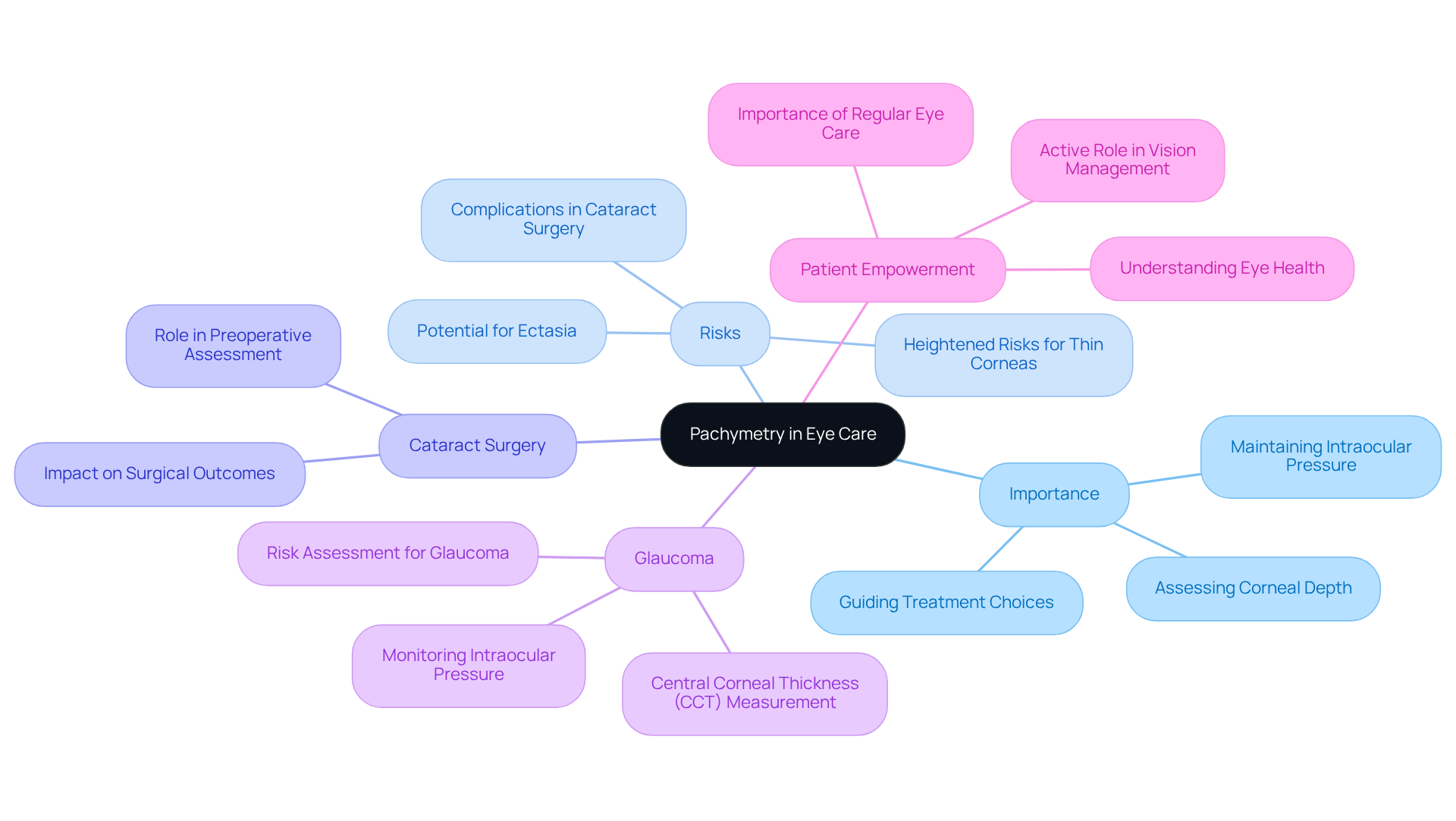
Define Pachymetry and Its Importance in Eye Care
Pachymetry is an essential diagnostic procedure that assesses the depth of the cornea, which is the transparent front surface of your eye. We understand that this measurement is especially vital for individuals . It helps assess the risk of complications and guides treatment choices, ensuring you receive the best care possible. Typically, a healthy eye layer varies from 540 to 550 micrometers, which is essential for maintaining intraocular pressure and overall ocular well-being. Research indicates that individuals with thinner eye membranes face heightened risks during surgical interventions, including cataract operations, as insufficient density can lead to issues like ectasia of the eye.
Understanding the importance of pachymetry empowers you to recognize its role in ensuring safe and effective cataract treatment. For instance, a case study highlighted the significance of measuring central ocular depth (CCT) in individuals over 50, greatly assisting in the early identification and treatment of glaucoma. It’s common to feel uncertain about these procedures, but specialists emphasize that measurements of the eye’s surface can significantly impact intraocular pressure readings, which are vital for diagnosing and monitoring glaucoma.
Recent studies underscore the connection between the depth of the eye’s surface and various ocular conditions, reinforcing the necessity for regular eye care that includes pachymetry. By acknowledging the importance of your eye’s layer density, you can take an active role in managing your vision health. This awareness ensures that you receive personalized care tailored to your specific needs. We are here to help you through this process, providing the support and information you need for your eye health journey.
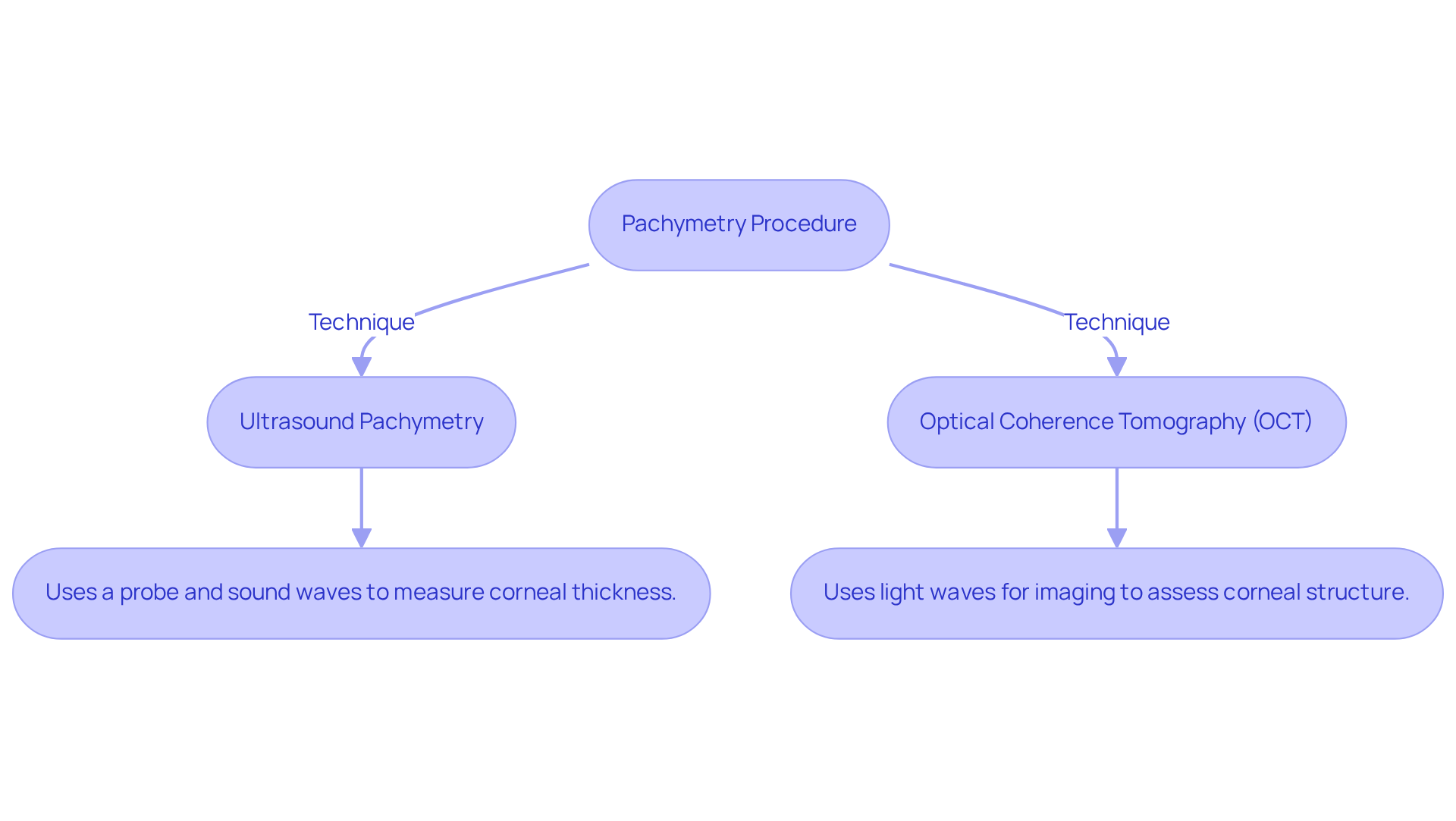
Explain the Procedure of Pachymetry: Techniques and Tools
Pachymetry is an essential procedure that can be conducted through various techniques, with ultrasound pachymetry and optical coherence tomography (OCT) being the most common options available.
- Ultrasound Pachymetry: This technique involves gently positioning a on the surface of your eye. It emits sound waves to assess the thickness of your cornea. The procedure is quick and painless, providing precise results that make it a reliable choice for evaluating your eye health.
- Optical Coherence Tomography (OCT): This non-invasive technique uses light waves to capture detailed cross-sectional images of your cornea. It allows for precise measurements without any direct contact. OCT is particularly effective in evaluating corneal structure and thickness using pachymetry, offering valuable insights for diagnosing conditions like glaucoma and keratoconus.
Both techniques are safe and usually completed within just a few minutes, ensuring minimal disruption to your day. We understand that learning about these procedures can feel overwhelming, but knowing about them empowers you to take an active role in your eye care. This fosters a sense of confidence and clarity regarding your treatment options, reminding you that we are here to help you through this process.
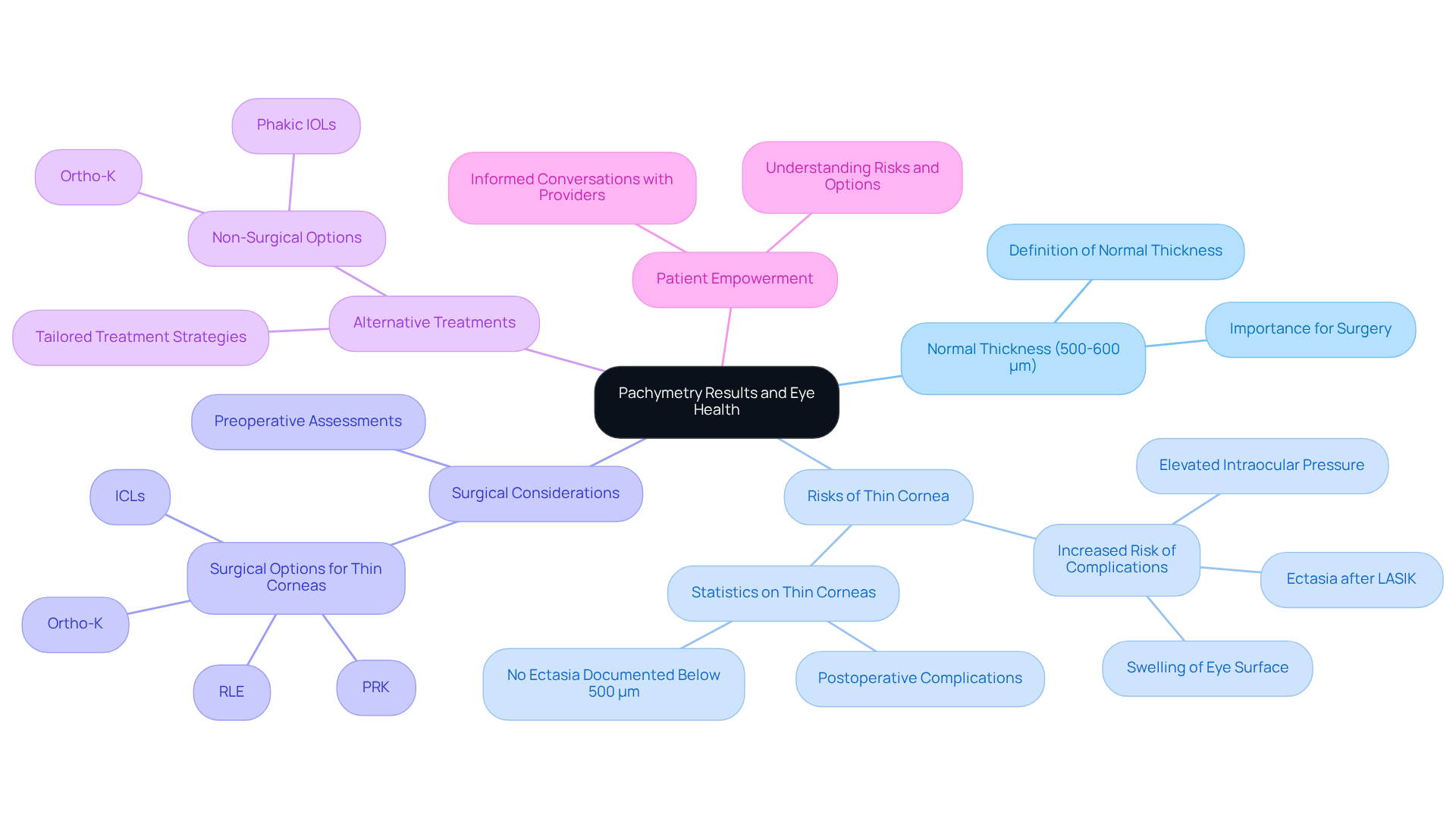
Interpret Pachymetry Results: Impacts on Eye Health and Treatment Decisions
The results of pachymetry are typically expressed in micrometers (µm), with a normal thickness of the eye surface ranging from 500 to 600 µm. We understand that measurements below this range may raise concerns about a thin eye surface, which can increase the risk of complications during cataract surgery. Specifically, patients with thin eye layers might experience elevated intraocular pressure and swelling of the eye surface. This situation requires careful observation and possibly different surgical methods to reduce these risks.
As Dr. J. Bradley Randleman notes, low preoperative corneal thickness, assessed through pachymetry, is a significant risk factor for complications, including ectasia after procedures like LASIK. This highlights the importance of , ensuring that you are well-informed about your options. Conversely, a thicker cornea may suggest conditions such as glaucoma, which can also influence the choice of surgical approach.
Comprehending these results empowers you to participate in informed conversations with your healthcare providers regarding your treatment choices and possible risks. For example, recent research indicates that individuals with a pachymetry measurement below 500 µm have a greater occurrence of postoperative complications. However, it’s reassuring to note that there have been no documented instances of ectasia in individuals with such measurements. This emphasizes the necessity for tailored treatment strategies based on unique eye profiles.
Furthermore, alternative methods like PRK and ICLs might be considered for individuals with thin corneas, offering effective vision correction without jeopardizing eye health. By prioritizing corneal health and thickness in surgical planning, you can enhance your chances of successful outcomes and recovery. Remember, we are here to help you through this process, ensuring that you feel supported every step of the way.
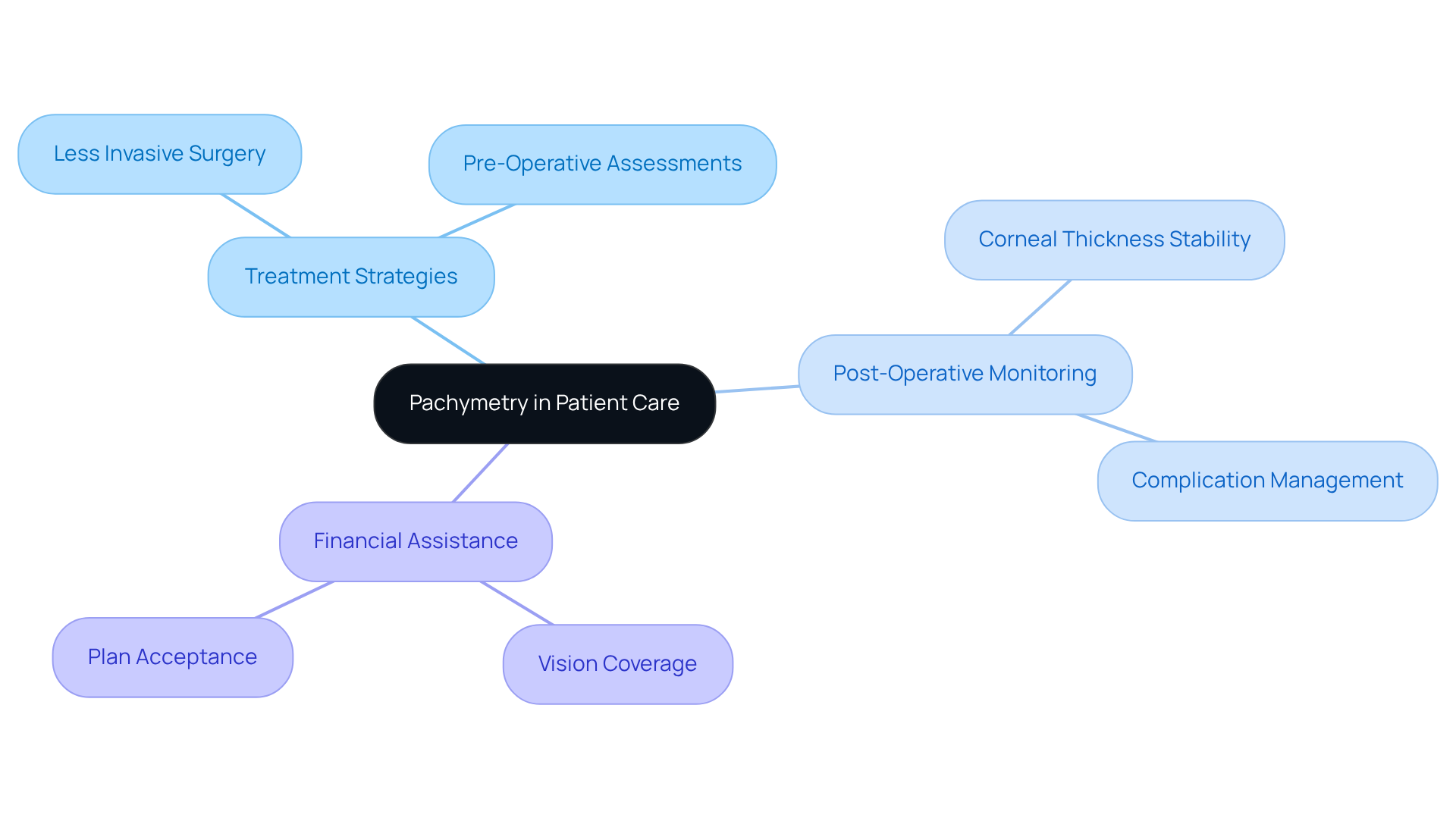
Utilize Pachymetry in Patient Care: Enhancing Treatment Strategies
Incorporating pachymetry into care at Northwest Eye enables our ophthalmologists to tailor treatment strategies effectively. We understand that concerns about eye health can be overwhelming. For instance, if you have a thin cornea, your surgeon may opt for less invasive cataract surgery techniques or additional pre-operative assessments to ensure your safety. This patient-centered approach is crucial in providing tailored to your individual needs.
Furthermore, pachymetry can be used to monitor individuals after surgery, ensuring that corneal thickness remains stable and that any potential complications are swiftly addressed. By utilizing pachymetry, our healthcare providers at Northwest Eye can improve outcomes for you, ensuring that you receive the most appropriate and effective care tailored to your specific needs. Additionally, understanding your vision coverage and plan acceptance can help you navigate financial assistance options for your cataract surgery, further supporting your journey to recovery.
Conclusion
Understanding the role of pachymetry in cataract care is crucial for ensuring optimal eye health and recovery. This diagnostic procedure not only measures corneal thickness but also plays a pivotal role in assessing the risks associated with cataract surgery. By becoming informed about the significance of pachymetry, you can take proactive steps in your eye care journey, leading to more personalized and effective treatment plans.
Throughout this article, we have explored key points, including the techniques used for pachymetry, such as ultrasound and optical coherence tomography, and their implications for patient care. The importance of interpreting pachymetry results has been emphasized, particularly in relation to surgical decisions and potential complications. This understanding empowers you to engage in meaningful discussions with your healthcare provider, ensuring that your unique needs are met during the treatment process.
Ultimately, recognizing the significance of pachymetry in cataract care extends beyond mere measurement; it is about enhancing patient outcomes and fostering a collaborative relationship between you and your healthcare professionals. By prioritizing regular eye examinations and staying informed about your eye health, you can navigate your cataract treatment with confidence, leading to a smoother recovery and a brighter future for your vision.
Frequently Asked Questions
What is pachymetry?
Pachymetry is a diagnostic procedure that measures the depth of the cornea, the transparent front surface of the eye.
Why is pachymetry important in eye care?
Pachymetry is crucial for assessing the risk of complications in individuals preparing for cataract surgery and helps guide treatment choices to ensure optimal care.
What is the typical measurement range for a healthy corneal layer?
A healthy corneal layer typically measures between 540 to 550 micrometers.
How does corneal thickness affect surgical risks?
Individuals with thinner corneal membranes face increased risks during surgical procedures, such as cataract surgery, as insufficient density can lead to complications like ectasia of the eye.
How does pachymetry relate to glaucoma?
Measuring the central ocular depth (CCT) is significant for early identification and treatment of glaucoma, especially in individuals over 50.
What impact do eye surface measurements have on intraocular pressure readings?
Measurements of the eye’s surface can significantly influence intraocular pressure readings, which are essential for diagnosing and monitoring glaucoma.
Why is regular eye care, including pachymetry, necessary?
Regular eye care that includes pachymetry is important for understanding the connection between corneal depth and various ocular conditions, helping to manage vision health effectively.
How can individuals take an active role in managing their vision health?
By recognizing the importance of corneal layer density and understanding pachymetry, individuals can engage in personalized care tailored to their specific eye health needs.